Breast elastography is an overlooked tool for evaluating breast cancer, especially since it shows promise for helping radiologists distinguish between benign and malignant lesions, according to a presentation delivered at the American Institute for Ultrasound in Medicine (AIUM) meeting in Orlando, FL.
Since ultrasound is convenient, easily accessible, and less expensive than some other modalities, it's a helpful tool in the breast cancer detection arsenal. And since it can help characterize breast lesions, breast elastography could have downstream effects on patient care, according to presenter Dr. Stamatia Destounis of Elizabeth Wende Breast Care in Rochester, NY.
"Identifying the relative tissue stiffness can help clinicians distinguish between benign and malignant lesions, which in turn has the potential to reduce unnecessary biopsies," she said.
Although breast elastography has been available for more than 15 years, it's not widely implemented, in part because the various methods lack consistency -- particularly in color scale interpretation, Destounis noted.
"As research continues and elastography is used in clinical practice, there's a need for standardization of the color scale," she said.
Elastography can be performed in static and dynamic modes, and consensus about which mode is better is generally lacking. Static elastography includes strain imaging, while dynamic elastography includes shear wave. Strain elastography is the most widely used technique, estimating the relative stiffness of a particular area compared with other tissue.
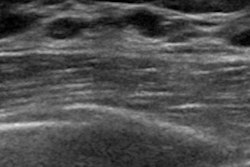
In strain elastography, tissue stiffness data are displayed in a color map that is superimposed on a real-time grayscale image. Cancers tend to appear larger on strain elastography than on B-mode ultrasound, and benign lesions tend to appear smaller; this size change between the modes has shown to be highly sensitive and specific for characterizing breast lesions, Destounis said.
Studies have demonstrated that strain elastography is effective for detecting breast cancer, but it does have its drawbacks.
"It can be difficult to measure the amount of force during compression, and absolute elasticity can't be calculated," she said.
As for shear-wave elastography, it offers real-time, quantitative assessment of tissue stiffness; rather than relying on external compression, it uses short acoustic pulses to identify stiffness. To characterize breast lesions, clinicians should focus on the area of highest stiffness in the lesion. But be careful, Destounis cautioned.
"Some breast cancers don't allow for adequate shear-wave generation and may appear black -- that is, no shear-wave speed calculated or with a low shear-wave speed due to noise," she explained.
So which technique should clinicians use? Destounis cited research from Chang et al that found mixed results (American Journal of Roentgenology, August 2013, Vol. 201:2, pp. W347-356). The study compared strain and shear-wave ultrasound elastography for differentiating benign from malignant breast lesions, and it showed that strain elastography is more specific than shear-wave elastography (93.7% compared with 84.8%) but less sensitive (81.7% compared with 95.8%).
It may be a matter of improving elastography technology, Destounis told AuntMinnie.com via email.
"Several vendors have different types of elastography technology, and it needs more consistency in technique and color representation," she stated.