A study conducted in Africa found that breast ultrasound can be used successfully by trained nurses and clinicians to detect lesions in areas where radiologists are scarce. The research was published June 20 in the Journal of the American College of Radiology.
A team led by Dr. Lydia Pace from Brigham and Women's Hospital in Boston found that nonradiologist clinicians at a hospital in rural Rwanda could evaluate lesions that proved to be cancer with high sensitivity and "acceptable" positive predictive value (PPV) and that "very few" lesions believed to be low risk were diagnosed as cancer.
"This suggests that diagnostic breast ultrasound capacity could be feasibly scaled up to district hospitals in Rwanda and similar settings, which could help decentralize a key aspect of breast cancer diagnosis and make services more accessible to patients," Pace told AuntMinnie.com.
Previous research suggests that two out of three breast cancer deaths occur in middle- and low-income countries. In these countries, screening mammography is not used as often and cancers are often diagnosed at a later stage.
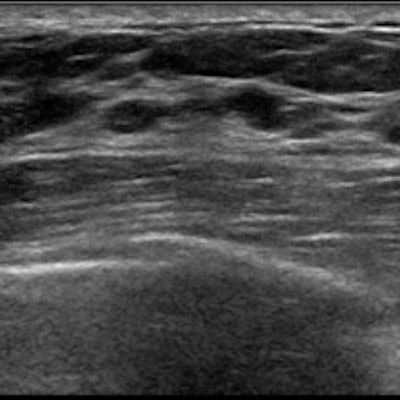
The study authors noted that breast ultrasound is considered to be safe and relatively inexpensive while being able to detect and characterize palpable lesions. They wrote that ultrasound can play a role in evaluating and triaging breast abnormalities, as well as determining whether biopsy is needed.
But radiologists are not widely available in rural areas in low-income countries, creating a barrier to access. Pace led a team that from 2015 to 2017 started a healthcare provider training program for early breast cancer detection in a rural part of Rwanda, the Burera District. The team's goal was to inform clinical protocols and build capacity in diagnostic breast ultrasound in Rwanda and other settings with limited resources.
The researchers trained nonradiologist doctors and nurses at the Butaro Cancer Center of Excellence, including seven weeks of intensive in-person training in January and February 2016, followed by e-mail remote supervision. Compared with trainer assessments, the sensitivity of trainee assessments for identifying a solid mass at medium or high suspicion of being cancerous was 95%, the authors wrote in a previous study at the center.
Pace and colleagues looked at data from 299 palpable breast findings from 199 patients, with 104 lesions initially biopsied. Out of the biopsied lesions, 38 were deemed to be malignant and three were deemed malignant on repeat biopsy.
A total of 34 patients were diagnosed with breast cancer and received initial recommendations for either biopsy or aspiration by trainees.
The team found that the positive predictive value of trainee biopsy recommendation was 34.8%, while their sensitivity for identifying malignant lesions was 92.7%. Of the 46 patients who did not receive biopsy and were told to return for clinical or imaging follow-up, 37% did not return.
The study authors wrote that none of the patients had subsequent diagnoses of cancer after being discharged or told to return for clinical or radiologic follow-up only. They added that all patients who were diagnosed with breast cancer received initial trainee recommendations for biopsy or aspiration.
The researchers also wrote that this information can be used to guide clinical protocols, such as thresholds for biopsy of benign-appearing lesions on ultrasound in limited-resource settings. "Where barriers to patient follow-up are high, lower thresholds for biopsy may be indicated, though these must be balanced with the costs and harms of unnecessary biopsies," they added.
Pace et al concluded that breast ultrasound is a "valuable" tool that is feasible and can expand access at health facilities in low-income countries.
"The World Health Organization's Global Breast Cancer Initiative is establishing recommendations for implementing breast cancer control, including rapid diagnosis, in resource-limited settings," they wrote. "Breast ultrasound performed by nonradiologists with adequate training and ongoing mentorship could play an important role in efficient evaluation of palpable masses."
Pace told AuntMinnie.com that with more sophisticated ways to teach virtually and share ultrasound images, the team would like to try some of these methods in the future as they work with Rwandan partners to scale up these efforts.