Fractional flow reserve (FFR) is noninferior to intravascular ultrasonography (IVUS) when it comes to evaluating patients for coronary artery disease, suggests a study published September 1 in the New England Journal of Medicine.
A team led by Dr. Bon-Kwon Koo from Seoul National University Hospital in South Korea found that using IVUS was tied to a higher frequency of percutaneous coronary intervention (PCI), as well as the use of more stents and more frequent administration of dual-antiplatelet agents than FFR.
However, patient-reported outcomes were similar when using both guidance strategies.
"The noninferiority of FFR guidance occurred with a lower incidence of target-vessel percutaneous coronary intervention in the FFR group than in the IVUS group, which led to the implantation of fewer stents and less frequent administration of dual antiplatelet agents," Koo and colleagues wrote.
Coronary angiography is the standard method for guiding intervention in coronary artery disease patients. Percutaneous coronary intervention is used to treat the narrowing of the coronary arteries of the heart found for this disease. However, various measurements are used for incremental information. This means other methods are used in addition to angiography, such as IVUS.
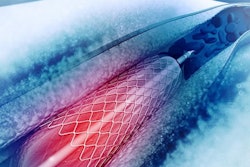
Images from IVUS can give clinicians anatomical information about the lumen, vessel, and plaque. It can also guide PCI to help with stent placement, minimize related problems, and improve patient outcomes.
FFR, meanwhile, involves the use of a pressure wire placed under interventional guidance to calculate the ratio between coronary pressure distal to a coronary artery stenosis, and it can help determine whether a stenosis is causing ischemia. Previous research suggests that FFR-guided interventions are tied to fewer clinical events than angiography-guided coronary interventions and medical treatment.
While both FFR and IVUS have their share of advantages, the study authors pointed out a lack of data comparing the two strategies when it comes to clinical outcomes. Koo and colleagues wanted to add to this, comparing both procedures head-to-head regarding clinical and patient-reported outcomes in patients with intermediate coronary stenosis.
The researchers at first wanted to prove FFR's superiority over IVUS. However, after the trial's start 2016, "several" studies showed that IVUS-guided stenting could further improve clinical outcomes, especially with the use of drug-eluting stents. Because of this, the Koo team modified their trial to explore the noninferiority of FFR-guided procedures in comparison with IVUS.
They looked at prospective data from 1,682 patients being evaluated for percutaneous coronary intervention for treating intermediate stenosis between 2016 and 2019. The patients had an average age of 65.1 years. Out of the total, 838 underwent the FFR-guided procedure while 844 patients underwent the IVUS-guided procedure.
The study authors found that clinical outcomes between the two groups were similar, indicating the noninferiority of FFR to IVUS. At 24 months, a primary-outcome event had occurred in 8.1% of the patients in the FFR group and in 8.5% of those in the IVUS group (p = 0.01 for noninferiority). The event in question was death from any cause, myocardial infarction, or revascularization.
Also, intention-to-treat analysis for the primary outcome in the FFR group was 8.2% compared to 8.7% in the IVUS group (p = 0.02 for noninferiority).
For patient-reported outcomes, characteristics at baseline showed close numbers between the two groups. A total of 519 patients in the FFR group had stable angina compared to 544 in the IVUS group, while 252 patients in the FFR group had acute coronary syndrome compared to 244 in the IVUS group.
At the same time, however, Koo and colleagues found that fewer patients were being referred for percutaneous coronary intervention in the FFR group. The frequency of PCI among all target vessels was 33.2% in the FFR group and 58.4% in the IVUS group. This led to the implantation of fewer stents and less administration of dual-platelet agents in the FFR group.
The study authors called for more research to help define the specific imaging and physiologic criteria for coronary intervention success, the relative importance of disease burden in non-stented segments, and profiles for patients and lesions that are tied to greater clinical benefit with adjunctive procedures.