An artificial intelligence (AI) decision-support system may help radiologists in diagnosing small invasive lobular carcinoma (ILC) on breast ultrasound images, according to research published May 16 in Clinical Imaging.
A team led by Dr. Tali Amir from Memorial Sloan Kettering Cancer Center in New York City found that their tested system demonstrated perfect accuracy in deeming imaging findings as suspicious or probably malignant.
"As AI evolves, the ability of a system to detect potential areas of interest on ultrasound for radiologist review may prove useful and help to decrease interval cancers in the setting of ILC," Amir and co-authors wrote.
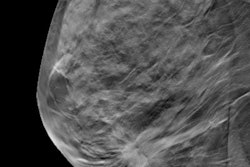
ILC can be challenging to detect since they show a variety of appearances on imaging. Previous studies found that for detecting these cancers, mammography has a sensitivity range between 57% and 81% while breast ultrasound has a significantly higher sensitivity range.
While breast radiologists are using AI to help with breast cancer diagnosis, the researchers noted that there is limited data on the technology's potential role in cases of invasive ILC.
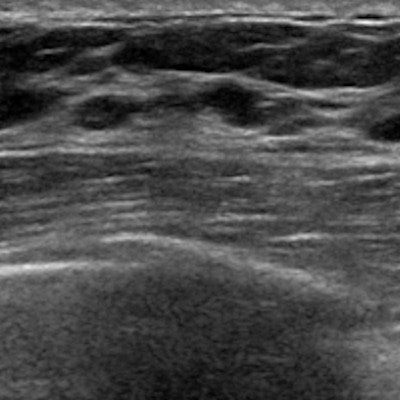
Amir and colleagues wanted to see how well an AI decision support system could perform in assessing ILC from breast ultrasound images. Using retrospective data, the team tested the system on 75 women with a total of 83 cases of invasive lobular carcinoma. These cases were diagnosed by core biopsy or surgery.
The researchers found that the AI decision support interpreted 100% of invasive lobular carcinomas in the study as suspicious or probably malignant. This included 100% sensitivity and a 0% false-negative rate.
The group also found that 82 of the 83 detected carcinomas were initially recommended for biopsy by the interpreting breast radiologist, and all were recommended for biopsy after one additional ILC was identified on same-day repeat diagnostic ultrasound.
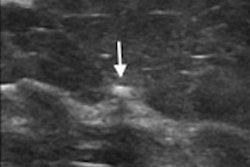
Additionally, lesions identified as probably malignant by the decision support, but assigned a BI-RADS 4 assessment by radiologists had a median lesion size of one cm. To compare, the median lesion size for BI-RADS 5 cases was 1.4 cm (p = 0.006). Finally, the team reported that 20% of patients with invasive lobular carcinoma were assigned a BI-RADS 5 assessment by the radiologist.
"These results suggest that AI may offer more useful decision support in smaller sub-centimeter lesions in which shape, margin status, or vascularity is more difficult to discern," the study authors wrote.
They added that future research should explore the impact of AI decision support on the confidence of radiologists in assessing and recommending for biopsy.