Point-of-care ultrasound (POCUS) may be useful in the emergency department for assessing and predicting severity for pediatric bronchiolitis, suggest findings published October 21 in the American Journal of Emergency Medicine.
Researchers led by Dr. Jaron Smith from the Children's Medical Center in Dallas found that higher lung POCUS scores for acute bronchiolitis are tied to increased respiratory support, longer hospital length of stay, and more acute disposition.
“These outcomes are of significant interest to the emergency department clinician managing a patient with acute bronchiolitis as lung ultrasound may provide an additional objective tool in assessment and prediction of disease severity,” Smith and colleagues wrote.
Acute bronchiolitis is the most common lower respiratory tract infection in infants, but its management can vary based on severity. This makes disease severity classification important, but current scoring tools are limited, the researchers noted.
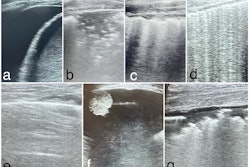
While imaging does not have a set role in diagnosing and assessing bronchiolitis, previous research has explored the potential of lung ultrasound in this area.
The Smith team sought to characterize lung findings on POCUS in infants presenting to the pediatric emergency department who are diagnosed with acute bronchiolitis. It also explored any associations between POCUS findings and respiratory support at 12 and 24 hours, maximum respiratory support during hospitalization, disposition, and hospital length of stay.
The researchers included data from 82 infants aged 12 months or younger. They found that the average lung ultrasound scores (range, 0 to 36, with lower scores equal to better outcomes) were 1.18 for discharged infants, 4.34 for those admitted to the floor, and 10.84 for those admitted to the intensive care unit (ICU).
The researchers also found that for respiratory support, average ultrasound scores were higher at 24 hours than at 12 hours.
Average lung ultrasound scores for respiratory support
| No respiratory support | Low respiratory support | High respiratory support | |
| 12 hours | 1.56 | 4.34 | 11.94 |
| 24 hours | 2.11 | 4.91 | 12.64 |
*All data achieved statistical significance.
The team also reported the maximum respiratory support ultrasound scores for the following: no support, 1.22; low support, 4.11; and high support, 10.45.
They also found that the mean differences for all dispositions and respiratory support time points were statistically significant. Finally, the team found that the average hospital length of stay was 84.5 hours, and the Pearson correlation coefficient comparing length of stay and lung ultrasound was 0.489 (p < 0.0001).
Despite their results, the study authors noted that it is not known whether lung POCUS scoring is as predictive as existing measures or how it compares to the gold standard of clinical assessment by a provider. They called for larger prospective studies to validate their findings.
However, the authors highlighted that lung POCUS could have value as an objective tool in assessing acute bronchiolitis severity.
The full study can be found here.