Contrast-enhanced ultrasound (CEUS) can improve locoregional therapy for treating metastatic disease of the liver, according to early study results presented April 10 at UltraCon.
In her presentation, PhD candidate Corinne Wessner from Thomas Jefferson University in Philadelphia, PA, highlighted initial findings from her team’s ongoing work suggesting that microbubble destruction from CEUS triggering is safe and well-tolerated among patients with intrahepatic cholangiocarcinoma (ICC) and metastatic liver disease who also receive transarterial radioembolization with yttrium-90 (Y90-TARE).
“When we add the ultrasound-triggered microbubble destruction, we’re increasing the tumor cell death, hopefully sensitizing these tumors,” Wessner said.
 Corinne Wessner from Thomas Jefferson University discusses early study results at UltraCon showing the potential of ultrasound-triggered microbubble destruction in treating liver disease.Amerigo Allegretto
Corinne Wessner from Thomas Jefferson University discusses early study results at UltraCon showing the potential of ultrasound-triggered microbubble destruction in treating liver disease.Amerigo Allegretto
ICC is a rare and aggressive epithelial cell malignancy that arises from the biliary tree in the liver. It consists of about 10% of primary liver cancers. Furthermore, metastatic disease to the liver is common in this area due to hepatic dual blood supply. The five-year relative survival rates tied to ICC are poor and variable, ranging from 11% to 42%, Wessner added. Furthermore, patients often present with the disease outside the criteria for surgical resection and transplantation.
Y90-TARE uses glass or resin beads containing Y90, providing a localized release of delivered doses ranging from 110-200 Gy to the tumor. However, Wessner pointed out that treatment efficacy is currently determined by a four- to six-month regimen with contrast-enhanced CT and/or MRI.
The researchers wanted to test the efficacy of CEUS microbubble-based radio-sensitization. Here, transient cavitation is activated via ultrasound-triggered microbubble destruction. This puts shear stress on the tumor endothelium and activates the production of ceramide, a radiosensitizer. The increase in ceramide leads to an increase in tumor cell death.
The study currently has nine enrolled participants, though Wessner said more are being recruited. The average tumor diameter recorded was 4.2 cm.
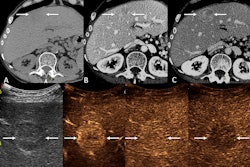
Wessner reported that no serious adverse events have been recorded among the participants and that out of five who have undergone follow-up exams, three have shown complete response with no internal enhancement two weeks after treatment.
She added that the lack of CEUS enhancement two weeks post-treatment correlated well, with no evidence of viable tumors on contrast-enhanced MRI and CT four to six months after Y90-TARE treatment.
Wessner called the results encouraging, saying the study demonstrates the potential of ultrasound-triggered microbubble destruction for liver tumor treatment.
“In the future, we’ll be looking at historical controls and matching them via propensity matching,” she added.