Radiofrequency ablation (RFA) can successfully treat malignant thyroid nodules with minimal adverse events, according to research published December 11 in Endocrine Practice.
A team led by Jennifer Kuo, MD, from New York Presbyterian Hospital – Columbia University in New York found that ultrasound-guided RFA achieved remission of hyperthyroidism in over four out of five patients with toxic adenomas or toxic multinodular goiters (MNGs).
“In our early experience, RFA is a safe and effective method for treating hyperfunctioning thyroid nodules of benign etiologies,” the Kuo team wrote.
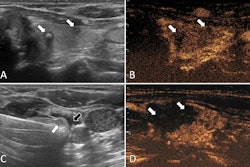
Image-guided RFA has grown in popularity among interventional radiologists and surgeons. Here, electrodes are inserted under ultrasound guidance to deliver thermal energy to targeted tissue, with only local anesthesia being used as a sedative. Surrounding healthy tissues meanwhile are spared and gradually fill in the area where RFA is targeted.
Proponents highlight the technique’s effectiveness and efficiency in treating patients within a shorter amount of time compared to conventional surgery. Previous studies suggest that RFA is also safe for patients, cost-effective, and can serve as a suitable alternative to surgery.
Kuo and colleagues use RFA at their institution. For the study, they reported their experience with the technique, focusing on its safety, effectiveness, and considerations in treating toxic adenomas and MNGs.
The study included data from 41 patients with symptomatic hyperthyroidism from toxic nodules. The patients chose to receive ultrasound-guided RFA, which was followed by imaging, laboratory studies, and clinical questionnaires. Two expert physicians performed RFA for the study cohort. The researchers recorded thyroid nodule volume via ultrasound at intervals of one, three, six, and 12 months post procedure.
By 12 months after RFA, solitary and multinodule lesions responded with an average volume reduction of 80.57%. Also, 35 of the total patients (85.4%) sustained remission from hyperthyroid state, achieving significant improvement in cosmetic and clinical symptoms.
Finally, the team reported nine total complications experienced by eight patients. Six patients experienced mild pain that did not require ending treatment, two had an infection after RFA treated by antibiotics, and one experienced a nodule rupture. The rupture was treated nonoperatively with antibiotics and drainage. However, no patients needed thyroid hormone supplementation following RFA.
The study authors highlighted that their results provide significant insight into RFA’s potential in treating thyroid nodules. They called for expanding their study population and more extensive follow-up to validate their findings and better characterize RFA outcomes as compared to other techniques.
“Future directions may also include a randomized control study comparing thermal ablation to surgical management of toxic thyroid nodules,” the authors wrote.
The study can be found in its entirety here.