The U.S. Centers for Medicare and Medicaid Services (CMS) has proposed that Medicare beneficiaries see a decrease in out-of-pocket costs for services from hospital outpatient departments (HOPDs) in calendar year 2011.
The proposed final rule from CMS updates payment rates and policies for services furnished in HOPDs and ambulatory surgical centers, and it implements changes required by the Affordable Care Act of 2010.
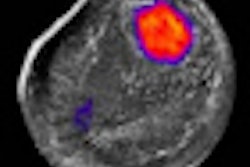
The Affordable Care Act waives beneficiary cost sharing for most Medicare-covered preventive services, such as screening mammograms and screening colonoscopies. For most preventive services, beneficiaries would not have to satisfy their Part B deductible before Medicare will pay.
In addition, beneficiaries will not have to pay their copayment for these services, which typically are 20% of the Medicare payment amount, for the physician's or the facility's portion of the service.
The final rule will appear in the November 24 edition of the Federal Register. Comments on provisions are due by 5 p.m. EST on January 3, 2011.
Related Reading
CMS issues final rule on preventive services, November 3, 2010
FDA, CMS propose parallel product review, September 20, 2010
CMS alters PET policy for treatment planning, August 6, 2010
CMS to offer EHR education series, July 29, 2010
CMS unveils imaging decision-support initiative, July 23, 2010
Copyright © 2010 AuntMinnie.com