Contrast-enhanced breast MRI is more accurate than whole-breast ultrasound in identifying extent of disease and contralateral lesions in women with newly diagnosed breast cancer, according to a study conducted by researchers at the University of Southern California in Los Angeles.
Finding the best imaging technique to estimate cancer size correctly is crucial, according to lead author Linda Hovanessian Larsen, MD, who presented her research at the recent RSNA meeting in Chicago. For women who choose breast-conserving surgery, underestimating the size and extent of cancer can cause them to undergo more -- and unexpected -- surgical intervention.
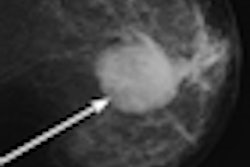
Targeted breast ultrasound has historically been used along with mammography for presurgical planning, but newer techniques, including breast MRI and whole-breast ultrasound, are showing promise. Larsen's group wanted to compare both techniques to the current standard of care.
"We wanted to identify which imaging technique -- bilateral MRI or bilateral whole-breast ultrasound -- when used in combination with mammography and targeted ultrasound would most accurately identify the extent of breast cancer, and additional tumor foci in the index breast and in the contralateral breast," she said.
Larsen's team compared three imaging arms, evaluating how accurately each measured tumor size, the impact on surgical treatment, and the identification of contralateral breast lesions:
- Standard of care (SOC): mammography and targeted ultrasound
- SOC combined with bilateral whole-breast ultrasound
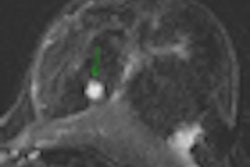
- SOC combined with bilateral contrast-enhanced breast MRI
The study included 271 women diagnosed with invasive breast cancer or ductal carcinoma in situ (DCIS) enrolled between September 2006 and September 2009. Each woman had a clinical breast exam, a diagnostic mammogram, a targeted breast ultrasound study, and a core biopsy of the index cancer as part of her initial evaluation. Each woman also had a bilateral MRI and bilateral whole-breast ultrasound in nonrandomized order; these exams were interpreted independently, but with clinical data available from the mammography, ultrasound, and biopsy, Larsen said.
Of the index cancers found, 86% were invasive ductal carcinoma and 14% were DCIS. The majority of breast tissue was characterized as scattered fibroglandular parenchyma, with dense breast tissue as the next most common type. More lesions were visualized with whole-breast ultrasound (90%) or breast MRI (86%) than with standard of care (75%).
With all tumor sizes, there was no significant difference in size of index lesion measured by mammography, ultrasound, and MRI, as compared to surgical pathology, Larsen said: Mammography found 70%, ultrasound found 71%, and MRI found 75%. Her team also found no significant difference in detection between mammography and MRI in terms of tumor size, although mammograms measured smaller tumors and MRI measured larger ones compared to surgical pathology.
For cancers larger than 30 mm, there were differences between the modalities, according to Larsen. MRI had a 56% detection rate, mammography had a 26% rate, and ultrasound had an 11% detection rate.
The study found 130 additional ipsilateral lesions in 98 women. Fifty-seven of these additional lesions were biopsied, and 21 were determined to be malignant. One of these 21 was found only by the SOC protocol, none were found by whole-breast ultrasound, and six (29%) were identified by MRI only.
"When we combined [standard of care] and MRI, all the malignant lesions were identified," Larsen said. "Ultrasound did not identify six of the malignant lesions, or 30%. And for 18 of these 21 women with malignancies, changes in management occurred, either wider excision or mastectomy."
The study also found 76 contralateral lesions in 61 women, of which 60 were biopsied; seven were found to be malignant and seven were categorized as high risk. Of these 14 malignant or high-risk lesions:
- SOC found six.
- SOC plus bilateral whole-breast ultrasound found nine.
- SOC plus MRI found 14.
"If we relied on standard of care only, we would miss a high-risk or malignant contralateral breast lesion in eight women," Larsen said.
As for surgical treatment, when MRI was included to evaluate the known cancer patient in addition to the standard of care, three times as many mastectomies were recommended than with standard of care and bilateral whole-breast ultrasound:
- SOC plus bilateral whole-breast ultrasound recommended breast-conserving surgery in 257 cases and mastectomy in 14.
- SOC plus MRI recommended breast-conserving surgery in 229 cases and mastectomy in 42.
Contrast-enhanced MRI is vital tool for identifying contralateral breast cancer, Larsen concluded.
"MRI, not ultrasound, should be used to evaluate the extent of disease and findings in the contralateral breast in women newly diagnosed with breast cancer," she said.
By Kate Madden Yee
AuntMinnie.com staff writer
January 12, 2011
Related Reading
Automated breast US system offers reproducible performance, December 1, 2010
Targeted breast US best for women under 30, November 22, 2010
Interactive breast ultrasound CAD improves lesion characterization, November 15, 2010
Shear-wave elastography improves ultrasound diagnosis of breast masses, November 12, 2010
'Multiple-bilateral' breast mass malignancy rate comparable to similar lesions, November 10, 2010
Copyright © 2011 AuntMinnie.com