Topics related to either diagnostic or therapeutic use of radiation dominated a top 10 list of important hospital technology topics for 2012, published this week by nonprofit technology research firm ECRI Institute.
ECRI's Top 10 C-Suite Watch List is designed to help hospital executives with their short- and long-term planning by helping them determine whether to adopt new technologies in the coming year. The report includes executive-level overviews of technology, and what ECRI calls its "unbiased perspective" on new technologies.
The top 10 list is as follows:
- Electronic health records
- Minimally invasive bariatric surgery
- Digital breast tomosynthesis
- New CT radiation reduction technologies
- Transcatheter heart valve implantation
- Robotic-assisted surgery
- New cardiac stent developments
- Ultrahigh-field-strength MRI systems
- Personalized therapeutic vaccines for cancer
- Proton-beam radiation therapy
A synopsis of the report's guidance on topics related to radiology and radiation therapy is provided below.
No. 1: Electronic health records
Unsurprisingly, ECRI found that the major issue faced by U.S. hospital executives regarding electronic health records is making sure that their health systems are certified to receive reimbursement for meaningful use under the American Recovery and Reinvestment Act (ARRA) of 2009.
ECRI advises executives to tackle the stage 2 certification criteria for meaningful use, which continues some stage 1 criteria while increasing the threshold for others, such as boosting the threshold for computerized physician order entry from 30% to 60%.
Stage 2 also requires hospitals not only to have the necessary IT infrastructure, but also the ability to integrate data from patient care devices, such as physiologic monitors and ventilators, into electronic health records, the report notes. Hospitals will need to develop device integration plans, which will require clinical engineering and IT staff to work together closely. Many hospitals also lack access to necessary information for medical device integration.
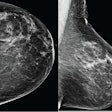
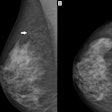
No. 3: Digital breast tomosynthesis
Hospitals are debating whether to purchase digital breast tomosynthesis (DBT) technology, with the first commercial DBT system, Selenia Dimensions from Hologic, approved in 2011, and the ECRI report notes that more DBT systems are on their way from other vendors. The group's analysis raises the question of whether it's advisable for the 22% of U.S. hospitals that aren't currently using 2D full-field digital mammography (FFDM) to jump directly to 3D DBT.
Not so fast, cautions ECRI. DBT doesn't replace traditional FFDM systems, it is additive; sites that adopt the technology should operate both 2D and 3D digital systems, the report advises. Initial data indicate that DBT can help radiologists identify cancer from benign tissue and reduce patient recalls: Manufacturer-sponsored studies found a 7% increase in radiologists' reading performance with DBT, and a 30% to 40% reduction in recalls. Data from multicenter trials are not yet available, however, nor is reimbursement for DBT exams, according to the report.
ECRI's analysis notes that DBT studies can double the radiation dose a patient receives because the 2D exam is still required (although manufactures are working to limit dose in cases where both 2D and 3D studies are performed). Reading 3D studies also requires additional training, and data storage costs can be higher as the technology adds another 50 to 60 images per patient.
ECRI advises that due to its novelty, DBT is probably best suited for sites "at the leading edge of technology use" and those that have considerable capital and operational resources. It noted that the challenges to implementing DBT, such as high capital costs and a lack of reimbursement, are "significant."
No. 4: New CT radiation reduction technologies
Reducing CT radiation dose has become the hottest topic in the modality, superseding the slice wars that previously dominated CT, according to the report. The primary focus has become optimizing scanning parameters for individual patients to reduce dose, rather than the "one-size-fits-all" approach used in the past for dose control.
A major development has been iterative reconstruction, which "seemingly achieves the impossible": lowering dose without reducing image quality, ECRI said. All major CT vendors now offer iterative reconstruction techniques, and the report states that its engineers determined in 2011 that the overall effectiveness of all the techniques is similar.
Iterative reconstruction was originally found only on premium CT scanners due to the cost of additional computing hardware; efforts to migrate the technology to lower-cost CT scanners have been slower, and vendors have been hampered by delays in getting U.S. Food and Drug Administration (FDA) 510(k) clearance because the agency is paying closer attention to dose-reduction claims. As a result, iterative reconstruction is available on more CT scanner models outside the U.S.
When considering iterative reconstruction, hospitals should evaluate image processing times because less costly versions compromise on the computer hardware used, the report states. A third-party alternative is available for scanners that don't have the option to upgrade to the technology.
The ECRI report also highlights the growing importance of dose monitoring and measurement. Several software options are becoming available to monitor and record dose -- these tools are just as important as scanner technology in efforts to control radiation dose, the report states.
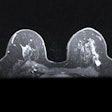
No. 8: Ultrahigh-field-strength MRI systems
In the past several years, MRI scanners using 3-tesla magnets have emerged, creating a new premium segment above the 1.5-tesla level that is the most common field strength in use, according to the report. While the new systems offer much better image resolution, they cost about $2.4 million, or $1 million more than a conventional 1.5-tesla scanner, and reimbursement is usually the same regardless of field strength.
The higher performance of 3-tesla scanners can be used either to boost image quality or decrease exam time -- but not both, the report notes. If used to reduce exam time, 3-tesla MRI can create workflow efficiencies for routine MRI studies, although more complex exams will take longer.
Other complicating factors can include additional staff training and expertise required to control for certain artifacts that are more common with 3-tesla scanning, and more attention should be paid to patient safety.
Over the past 10 years, studies comparing 3-tesla MRI to less powerful scanners have found better image quality at the higher field strength, and increased confidence in lesion detection, the report notes. "But the clinical value of these advances is difficult to gauge," according to ECRI, because most comparative studies have not assessed patient outcomes.
With that in mind, 3-tesla MRI research has focused on new clinically useful information that can be gleaned with the scanners, such as in neurological applications, while there's little evidence that 3-tesla MRI is necessary or improves patient outcomes for other uses, the report states.
ECRI concludes its analysis by advising hospitals that while 3-tesla image quality is better, the technology has drawbacks that potential purchasers should consider. It advises sites with neurosurgery programs to seriously consider acquiring 3-tesla MRI, but such a purchase may be harder to justify for facilities that focus on routine applications.
No. 10: Proton-beam radiation therapy
This new radiation therapy technology uses proton beams rather than the traditional photon beams as a source of radiation for treating cancer. The difference is that protons have the theoretical ability to deliver high-dose radiation to a tumor with little damage along the route of the beam, the ECRI report states. This creates the potential to reduce acute and long-term side effects of radiation therapy.
The downside to proton therapy is the cost. The technology requires the construction of custom-built particle accelerators, either cyclotrons or synchrotrons, and a cyclotron can weigh up to 240 tons and cost $100 million or more. The total cost of a proton-beam therapy center with five or six patient vaults approaches $200 million, the report notes. Once a center is built, operation and maintenance costs can reach $20 million to $25 million annually.
There are currently at least 33 proton therapy facilities in operation worldwide, with 20 more under construction or in the planning stages. The U.S. currently has nine centers, with that number expected to rise to 15 by 2013, according to ECRI.
The report states that while proton treatments are estimated to be three times as expensive as state-of-the-art photon-based therapy, the U.S. Centers for Medicare and Medicaid Services (CMS) budgeted a 15% increase in payments for 2012. Most reimbursement is at the discretion of local carriers, however.
There are no available comparative effectiveness data for proton therapy versus photon therapy, nor are there any randomized clinical trials under way in the U.S., ECRI noted. Proton therapy may also face competition from carbon ion therapy centers, which are just as expensive but are being adopted in Europe and Japan.
"Facilities planning to adopt this technology should carefully consider the high cost, limited evidence, and uncertain reimbursement climate before making a decision," the report concludes.