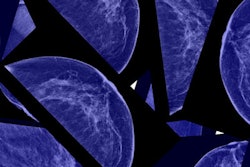
Mammography-detected breast cancers are found earlier, with reduced mortality in women between the ages of 40 and 49, according to a study in the March issue of Radiology. The study adds another dimension of benefit for women and their doctors to consider when making the decision to participate in a screening program at a younger age.
Researchers at the Swedish Cancer Institute in Seattle determined that by finding cancers earlier, women undergo less invasive treatment (Radiology, March 2012, Vol. 262:3). The findings add more data to the debate concerning the balance of harms and benefits regarding mammography screening at age 40, sparked in 2009 by a U.S. Preventive Services Task Force (USPSTF) recommendation which advised that younger women should not participate in annual mammography screening due to the "harms" that derive from screening.
"The ... U.S. Preventive Services Task Force found at least fair evidence that mammography screening can improve health outcomes but concluded that the balance of benefits and harms is too close to justify a general recommendation," wrote lead author Judith Malmgren, PhD, and colleagues. "[But this recommendation] was based on a computer modeling analysis of randomized, controlled trials carried out predominantly in the past century."
The goal of Malmgren's study was to assess the differences between breast cancer detected by mammography versus when symptoms appear. The group also wanted to determine whether earlier detection confers a treatment and morbidity advantage because the disease is found at an earlier stage.
"I appreciate the USPSTF looking at the issue," Malmgren told AuntMinnie.com. "But I think the harms of screening mammography are getting overemphasized and the benefits are not being fully described. Our study adds a more thorough description of the benefits."
Malmgren's team reviewed breast cancer patient information from a dedicated registry at the Swedish Cancer Institute's community cancer center, analyzing data on 1,977 breast cancer patients between the ages of 40 and 49 who were treated between 1990 and 2008. The group reviewed method of diagnosis (detected by mammography, patient, or physician), stage at diagnosis (0 to IV, confirmed by biopsy), treatment, and annual follow-up information, including recurrence of disease.
The researchers found that women with cancer detected by mammography were less likely to die of breast cancer (4% versus 11%). The analysis also revealed a significant increase in the percentage of mammography-detected breast cancer over the 18-year period, from 28% in 1990 to 58% in 2008. Over the same period, patient- and physician-detected breast cancer declined from 73% of all cases in 1990 to 42% in 2008.
Malmgren's group also found that the number of stage 0 breast cancers increased by 66% over the 18-year period, while the number of stage III breast cancers decreased by 66%. The majority of stage 0 cancer cases were ductal carcinoma in situ (DCIS).
Earlier detection translated to less invasive treatment, the team found: Compared with women whose cancer was self-detected or discovered by a physician, patients whose cancer was detected using mammography were more likely to have breast-conserving treatment and less likely to have chemotherapy. Specifically, women with cancer detected by mammography were more likely to undergo lumpectomy (67% versus 48%), and less likely to undergo modified radical mastectomy (25% versus 47%).
"The objective is to find disease when it's more treatable," Malmgren said. "It's the medical community's challenge to deal with byproducts of screening such as finding DCIS. We shouldn't stop screening because it's traumatic [to find this type of lesion]. It's pretty traumatic to die of cancer, too."
Frosting on the cake
Malmgren's study specifically addresses issues promulgated by a "small, but vocal group of individuals who have been trying to reduce access to mammography screening for several decades" -- including the arguments that screening is of little benefit for women ages 40 to 49, screening does not lead to a decrease in more advanced cancers, and screening results in an increase in more mastectomies, said Dr. Daniel Kopans of Massachusetts General Hospital.
"This paper by Malmgren et al in Radiology specifically addresses these issues and shows them to be belied by the facts," Kopans told AuntMinnie.com by email. "The authors provide strong evidence in their longitudinal analysis of breast cancers in their referral center over time that women ages 40 to 49 undergoing screening have had an improvement in the size and stage of their cancers that has translated into fewer deaths; as screen-detected cancers increase, the percentage of advanced breast cancers decrease; and that mastectomy rates decrease with an increase in screen-detected cancers."
However, there are potential biases in studies such as this one, Kopans said.
"It is important to remember that observational studies are 'frosting on the cake': They cannot be used to prove the benefit of screening," Kopans said. "This can only be done with randomized, controlled trials. But [studies like this one] do show what happens when screening is introduced into the population, and they support the results from the randomized, controlled trials."
What about DCIS?
The study implies that the 2009 USPSTF recommendations against routine annual screening mammography for women in their 40s were wrong, according to Dr. Leonard Berlin, professor of radiology at Rush University and the University of Illinois in Chicago. But the study's findings may be confounded by the DCIS cancers included in the cohort, he said. Because DCIS is usually found only by mammography, if those cases had been removed from the dataset, the relative survival rates between the two groups (women whose cancer was detected by mammography, compared with women whose cancer was detected by palpation) might be comparable.
"I do wonder about certain issues that are not discussed completely, specifically DCIS," Berlin told AuntMinnie.com. "Virtually every case of DCIS is diagnosed by mammography because of its characteristic mammographic calcifications -- DCIS almost never presents as a palpable lump or mass. Therefore, [including DCIS cases] skews the authors' findings in relation to tumor size and stage of disease when the cancer is initially diagnosed."
The exact percentage of untreated DCIS cases that progress to invasive cancer is unknown, but many authorities believe that it is probably in the 50% range. Because clinicians are unable to determine which DCIS patients should and should not be treated, virtually 100% will receive treatment, Berlin said.
"The authors appropriately state that patients should be empowered to make their own decisions as to whether to undergo screening mammography by being counseled in regard to the benefits and harms of screening mammography," he said. "But I wonder how many patients are informed that very likely one-half of women with DCIS will receive treatment -- chemotherapy, radiation, lumpectomy, mastectomy -- for a 'disease' that would never have harmed them in any way, and but for having undergone screening mammography, they would never have known they had?"