Digital breast tomosynthesis (DBT) when used as a screening tool for breast cancer reduces recall rates by 37% and increases the detection of invasive cancers by 54%, according to a new study published online May 22 in the American Journal of Roentgenology.
Researchers from TOPS Comprehensive Breast Center in Houston found that using digital breast tomosynthesis (Selenia Dimensions, Hologic) in its screening practice resulted in a consistent improvement in performance, including a doubling of the positive predictive value (PPV) of recalls. The results specifically address a number of concerns expressed by critics of screening mammography, according to lead author Dr. Stephen Rose.
 Dr. Stephen Rose from TOPS Comprehensive Breast Center.
Dr. Stephen Rose from TOPS Comprehensive Breast Center.
"I expected that we would see reduction in recall rates, but was surprised at the level of increase in cancer detection," Rose told AuntMinnie.com. "We saw a 54% increase in invasive cancer detection and a 35% increase in overall cancer detection. And one of the other surprises was that our positive biopsy rate went way up."
Rose and colleagues used procedure outcome-related databases to evaluate recall, biopsy, and cancer detection rates, and they calculated PPVs in the clinical breast imaging practice before and after the introduction of tomosynthesis for routine screening mammography. In all, 13,856 women received 2D screening mammography studies without the use of tomosynthesis, while 9,499 women underwent both 2D and 3D mammography. Images were interpreted by six radiologists, and their performance with the two protocols was analyzed (AJR, May 22, 2013).
Tomosynthesis lowered the recall rates for the six radiologists, from 8.7% for mammography alone to 5.5% for mammography interpreted with DBT. Adding tomosynthesis also improved four of the six radiologists' individual recall rates as well. The team also reported the following:
- An 11% drop in biopsy rate, from 15.2 biopsies per 1,000 screenings without tomosynthesis to 13.5 with DBT
- A 35% increase in the overall cancer detection rate, from 4.0 per 1,000 screenings without tomosynthesis to 5.4 per 1,000 screenings with the technology
- A 54% increase in the invasive cancer detection rate, from 2.8 per 1,000 screening examinations without tomosynthesis to 4.3 with it
- An increase in the positive predictive value for recalls, from 4.7% without tomosynthesis to 10.1% with the technology
Are these improvements simply the result of adding a new modality into the clinical mix? No, according to Rose and colleagues.
"One could argue that some or all of the reduction in recall rates and improvement in detection rates we observed for the high-volume radiologists may be attributable simply to the introduction of an additional modality (tomosynthesis) and therefore may not persist over time," they wrote. "However, the magnitude of the simultaneous changes we observed for both recall and cancer detection rates, particularly invasive cancers, suggests that the underlying technology is indeed aiding the radiologists."
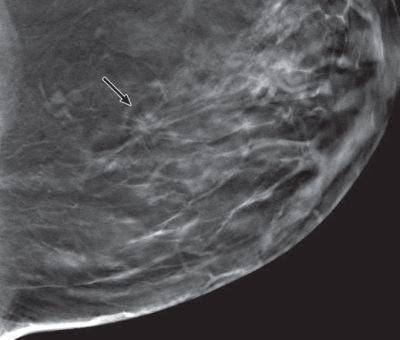
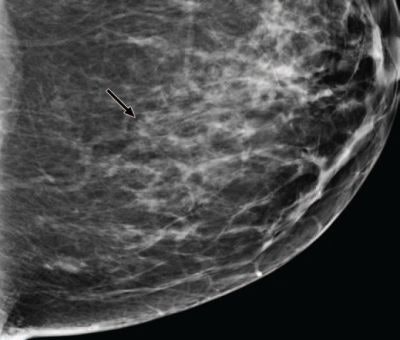 Comparison of digital mammography and tomosynthesis images in 42-year-old woman with 10-mm invasive ductal carcinoma in left breast. Craniocaudal images for digital mammography (above) and tomosynthesis (below). All clinical images courtesy of AJR.
Comparison of digital mammography and tomosynthesis images in 42-year-old woman with 10-mm invasive ductal carcinoma in left breast. Craniocaudal images for digital mammography (above) and tomosynthesis (below). All clinical images courtesy of AJR.
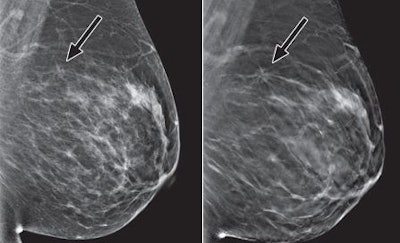 Mediolateral oblique images for digital mammography (left) and tomosynthesis (right). All tomosynthesis images show improved visibility of cancer (arrow) and cancer margins compared with digital mammography.
Mediolateral oblique images for digital mammography (left) and tomosynthesis (right). All tomosynthesis images show improved visibility of cancer (arrow) and cancer margins compared with digital mammography.Addressing 'harms'
So how might these findings influence the current debate over screening mammography's efficacy -- and its potential harms of overdiagnosis and false-positive biopsies? The increased PPV for recalls and biopsies suggests that tomosynthesis may address these issues, even for younger women, according to the authors: The study showed a large reduction in recalls for women in all age groups, including those younger than 50 years.
"These findings should put the controversy to rest," Rose told AuntMinnie.com. "I'm not saying they will, but they should. If you're going to reduce false positives by 40% to 50% and increase invasive cancer detection by the same percentages, arguments against screening mammography become much more difficult to maintain."
Remaining roadblocks
Digital breast tomosynthesis does take more time to interpret, and it does give a woman double radiation exposure because 2D images are acquired before the 3D images, according to Rose. That said, Hologic has received clearance from the U.S. Food and Drug Administration (FDA) for software that generates 2D images from the 3D data acquired during the exam. Because this software will eliminate the need for the 2D exposure, it will reduce a woman's radiation dose, he said.
"The 2D software is another step up," he added.
The biggest challenge to tomosynthesis is financing the technology and getting reimbursed for it, according to Rose. If a center has just recently upgraded to 2D mammography, it won't have had time to amortize that investment. And Medicare currently does not pay for tomosynthesis.
"We're going to have to push the powers that be to get a CPT code," he said. "Right now, it's based on 2D reimbursement, although we do use the miscellaneous code and are sometimes reimbursed for 3D."
Too good to be true?
The study results suggest that 3D breast imaging isn't just for diagnostic mammography -- its real power is for screening, Rose said.
"Our results sound too good to be true, and I'd say that if I wasn't in the middle of [this research]," he said. "This isn't a fluke. Tomosynthesis could be the best thing that's ever happened to breast imaging."
Study disclosures
Dr. Stephen Rose is a speaker and consultant for Hologic.