Managing high-risk breast lesions with no consensus can be tricky, but breast radiologists can navigate this area, according to a presentation given April 29 at the American Roentgen Ray Society (ARRS) annual meeting in San Diego, CA.
Amie Lee, MD, from the University of California, San Francisco, outlined several common types of high-risk breast lesions and what recent studies have found about best practices in managing them, from surveillance imaging to surgery.
“Now, it’s a lot more nuanced, with a growing trend toward less aggressive, nonoperative management,” Lee said.
Historically, healthcare has turned to surgery for treating most high-risk breast lesions diagnosed at core needle biopsy. However, with precision medicine at the fore, radiologists are exploring less invasive options for individual patients to mitigate unnecessary or low-value procedures.
But medical societies have different recommendations for managing these lesions, owing to the conflicting literature. For example, the National Comprehensive Cancer Network recommends surgical excision for atypical ductal hyperplasia (ADH). However, the American Society of Breast Surgeons recommends that if the entire ADH is excised on core needle biopsy, observation can be performed based on risk factor assessment and multidisciplinary input.
With no consensus to lean on, the radiologist-pathologist correlation becomes more important for image-guided breast biopsies.
“You are not ‘done’ with your biopsy until you have assessed concordance and issued a management recommendation,” Lee said.
Lee added that core needle biopsy may underestimate disease and may sometimes upgrade to malignancy at excision. And diagnosis may be tied to a higher future incidence of breast cancer.
Papillary lesions
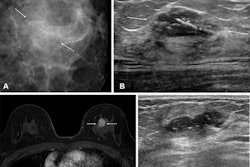
On mammography, papillary lesions present as round or oval masses and may or may not have associated calcifications. On ultrasound, they present as masses, sometimes within the dilated duct. These masses are complex and cystic, having internal vascularity.
While many papilloma lesions are benign or present with atypia, some can progress to ductal carcinoma in situ (DCIS) or malignant lesions. Adding to the challenge, papillary masses can be heterogeneous, having both benign and malignant components. This makes these lesions suspect to sampling errors.
Lee said that papillary lesions with atypia should be surgically excised, citing the higher risk of undersampling. However, papillary lesions without atypia have upgrade rates ranging from 0% to 33%. Lee said the current trend leans toward less excisions, with recent prospective studies suggesting an upgrade rate of 2% or less.
Radial scars
Radial scars are stellate lesions with a fibroelastic core, 1 cm or less in size. Larger lesions are referred to as complex sclerosing lesions. On mammography, they present as architectural distortions. On ultrasound, they present as masses with irregular shadowing and have no sonographic correlate.
While these lesions have historically been recommended for surgery, with a 0% to 40% upgrade rate, recent trends have shown lower upgrade rates with good biopsy sampling. These architectural distortions are seen more on digital breast tomosynthesis (DBT), lowering the modality’s positive predictive value.
Lee cited recent studies that suggest surveillance imaging is the go-to route for managing radial scars without atypia.
Atypia
Lee outlined three types of atypia in her presentation: atypical ductal hyperplasia (ADH), flat epithelial atypia (FEA), and lobular neoplasia (atypical lobular hyperplasia [ALH] and lobular carcinoma in situ [LCIS]).
There is no consensus for standard management of atypia, with studies showing conflicting and wide ranges in upgrading. This makes for wide variation in management, even among institutions, Lee said.
ADHs are the most common biopsied high-risk lesions, presenting mostly as calcifications on imaging. While they are small in size (2 mm or less), they carry a high risk of underestimation.
With an average upgrade rate of 23%, Lee said surgical excision is the best option for ADHs. However, she added that future prospective studies could help determine who may be best for surveillance or chemoprevention.
FEAs, meanwhile, have an upgrade rate of 0% to 21%, with Lee noting a lack of large studies on these lesions. The ASBrS suggests observation for FEAs, though surgery can be performed if there is concurrent ADH.
One study that Lee cited, published in 2025, found FEA upgrade rates were 4.7% based on local pathology review and 1.3% based on central pathology review. It also suggested that management should be based on shared decision-making.
 Amie Lee, MD, presented at ARRS 2025 on managing "controversial" high-risk breast lesions diagnosed on core needle biopsy. This slide outlines how to manage pleomorphic lobular carcinoma in situ (LCIS) via surgical excision.ARRS
Amie Lee, MD, presented at ARRS 2025 on managing "controversial" high-risk breast lesions diagnosed on core needle biopsy. This slide outlines how to manage pleomorphic lobular carcinoma in situ (LCIS) via surgical excision.ARRS
Lobular neoplasia is most often an incidental finding on core needle biopsy without imaging features. These serve as risk markers for future invasive cancer development. However, the risk of cancer is bilateral and not always near the core biopsy site, Lee said.
A 2016 study she cited found an upgrade rate of 1.3% for lobular neoplasia after central pathology review. Lee said that observation can be performed for these lesions, with the exception of LCIS variants like pleomorphic LCIS, which should be excised.
AI and imaging tools
AI is one tool that radiologists have been exploring for differentiating between breast lesions that require surgery and lesions that can be observed.
Lee cited a 2017 machine learning study of over 1,000 high-risk lesions, which found an upgrade rate of 11.4%. About 31% of surgeries of benign lesions would be avoided from the machine learning model’s predictions, with 97% of malignancies being diagnosed at excision, the study also found.
“This study suggests that machine learning holds promise in guiding surgical decision-making,” Lee said. “It’s a promising proof-of-concept study, but not ready for clinical use.”
Lee also highlighted MRI’s high negative predictive value in identifying high-risk lesions like ADHs and radial scars that can undergo nonsurgical management. She cited a 2023 retrospective study showing a 16% upgrade rate for ADHs by MRI, with all upgraded lesions presenting as enhancements. Images with no enhancement had a 0% upgrade rate in the study.
“Lack of enhancement of these high-risk lesions could potentially allow for deferral of surgical excision,” Lee said.