Researchers from the University of Michigan have developed a new double-barreled approach to computer-aided detection (CAD) that uses two separate CAD algorithms on digital breast tomosynthesis (DBT) exams. They believe the technique enables a high level of sensitivity with lower radiation dose.
The technique applies independent CAD algorithms to analyze microcalcifications in mammography images: first to data acquired with a modified low-dose DBT protocol, and then to a planar projection image derived from the DBT data. With their approach, the researchers achieved a high level of sensitivity while cutting radiation dose in half -- to the level of a conventional full-field digital mammography exam, according to Ravi Samala, PhD, who presented the study results at RSNA 2014.
Using two CAD algorithms is key to the process because it takes advantage of the lower radiation level in the modified low-dose DBT technique, while providing the opportunity to view the same breast microcalcifications from different angles.
"There is potential to combine these two systems to increase overall sensitivity," Samala said.
Prototype DBT unit
The group started with a prototype DBT system (GEN2, GE Healthcare) that was used to obtain two-view (craniocaudal and mediolateral oblique) images in 154 breasts. Images were then processed to simulate two types of DBT acquisitions, a normal protocol and a low-dose protocol.
In normal operation, the GEN2 system acquires 21 projection angles spanning 60° in 3° increments, with a scan time of less than eight seconds. The system has a step-and-shoot design that leaves both the x-ray source and detector stationary during exposure, Samala said. The total radiation dose of this mode is equivalent to two FFDM acquisitions.
For the lower-dose exam, the researchers developed a technique that uses a subset of the DBT system's normal acquisition protocol, with 11 projection views acquired in an arc of 30°. This cuts radiation in half, generating a dose comparable to that of a single FFDM scan.
The researchers then moved on to the CAD portion of the study. To create a second dataset in addition to the DBT data for CAD analysis, Samala and colleagues created what they called planar projection (PPJ) images from the DBT data in both 60° and 30° modes. PPJ images were developed through a series of image processing steps that emphasized high-frequency bands in the DBT dataset, which are where microcalcifications tend to be found. Maximum intensity projection processing was then applied to the high-frequency data to produce a final PPJ image.
Finally, two independent CAD algorithms, both developed at the University of Michigan, were applied separately to the DBT and PPJ images to detect microcalcifications. The researchers then compared the effectiveness of the dual-CAD approach in both the normal-dose 60° and lower-dose 30° datasets.
The study population consisted of 154 breasts, including 116 breasts with microcalcifications (34 malignant, 82 benign) and 38 without microcalcifications. The volumes were divided into a CAD training set of 64 breasts with clusters of microcalcifications, and a CAD test set of 52 breasts with microcalcifications and 38 without.
Significant improvement
The results showed that the value of the two CAD systems was additive. Running the two CAD algorithms on the low-dose 30° DBT and PPJ images delivered 85% sensitivity for microcalcification clusters, with 1.72 false positives per DBT volume by view, and 0.49 false positives per DBT volume by case, Samala said.
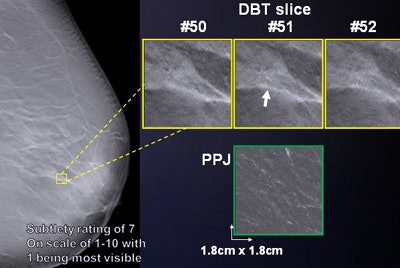 DBT CAD detected a microcalcification, while the planar projection CAD image shows no abnormality. Image courtesy of Ravi Samala, PhD.
DBT CAD detected a microcalcification, while the planar projection CAD image shows no abnormality. Image courtesy of Ravi Samala, PhD.In fact, running the dual-CAD protocol on the low-dose DBT and PPJ images was comparable to applying individual CAD to either the DBT or PPJ images derived from normal-dose 60° studies, both of which had 85% sensitivity -- but at twice the radiation dose.
In addition, the dual-CAD protocol applied to low-dose DBT and PPJ images was better than a single CAD algorithm applied to either low-dose DBT images (which produced 74% sensitivity) or low-dose PPJ images (which produced 79% sensitivity) -- differences that were statistically significant.
The researchers concluded that joint CAD on low-dose DBT and PPJ images provided a statistically significant improvement over a single CAD protocol at a low dose, while providing comparable performance at half the radiation dose to a dual-CAD protocol at a normal dose.
Regarding study drawbacks, Samala said that noise remains a major factor degrading microcalcification detection. More effective regularization methods need to be developed for reconstructing DBT images.



















