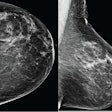
More money is paid out for breast cancer claims than for any other form of medical negligence, at $297 million per year, and radiologists are involved in 43% of these claims, according to a presentation at the National Consortium of Breast Centers (NCoBC) meeting in Las Vegas. So how can a breast center manage this risk?
With nurse navigators, said presenter Gerald Kolb, president of the Breast Group in Bend, OR, and consultant to breast imaging software developer Volpara Solutions.
"Navigators have a very important role in the care of individual patients, but they can also be a force for excellence in the breast center," he concluded. "And excellence is the ultimate mitigator of medical-legal risk."
What is a navigator?
The concept of a patient navigator was developed by surgeon Dr. Harold Freeman at Harlem Hospital in New York City nearly 30 years ago. It is now a well-established form of support for patients. Navigators understand the trajectory of individual cancers and are in touch with the day-to-day impact of the disease on patients, according to Kolb. They're helpers who are trained to ease the effects of breast cancer on patients beyond purely clinical approaches.
"For many patients, a cancer diagnosis throws them into an emotional, physical, and social whirlwind. Proceeding through a course of care could be a very daunting task, so a nurse can act as a liaison between the patient and healthcare team," Kolb said. "A nurse navigator can provide individualized support, including appointment facilitation, communication with physicians, and support during treatment and recovery, and can act as a source for education and advocacy."
Risk management
So what kinds of risk can patient navigators help manage? Many, according to Kolb, including what he calls the "triad of error" of claims for missed diagnosis of breast cancer: women between the ages of 30 and 49, women with self-discovered breast masses, and mammograms originally interpreted as normal.
Another key part of managing malpractice risk is how health information is gathered and used, Kolb said. Breast center navigators interact with multiple physicians involved in an individual patient's care, as well as with the patient's family and friends. Kolb suggested that navigators keep a log of when and what type of patient information has been released, and to whom.
"Protected health information concerns the health status, provision of care, and payment for care for an individual," he said. "Navigators have access to more of this information than anyone in the breast cancer care continuum. But just because a breast center operates with a common vision and mission doesn't mean that this information can be shared within the center."
Kolb gave three suggestions for ways breast center patient navigators can help manage malpractice risk:
- Demand quality. "Quality is the first line of defense against risk, and it happens by design, not by accident," he said. Establish and use quality metrics, such as from the National Accreditation Program for Breast Centers (NAPBC) or the National Quality Measures for Breast Centers (NQMBC). Don't accept anything less than excellence. Missing or sloppy reports or other documents will expose your center to malpractice risk.
- Document everything. "Missing documents that are to be expected in the medical record will be subject to comment if you have to go to court," Kolb said. "Inconsistent patterns of documentation are suspect. Be concise, check your work -- a recent study found errors in almost 50% of computer reports -- and do not use texting shortcuts. 'LOL' is not a medical term."
- Mind your Ps. "One of the first things investigators request when something goes wrong is the policy manual," he said. "Quality care is established by process, which is linked to good policy. Risks are largely exceptions to process. Finally, protocols are your clinical policies, and evidence-based ones will tend to contain medical-legal risk."
Help for the helpers
For patient navigators to function well, they also need support, Kolb said. Without it, burnout rates are high -- and the risk of HIPAA violations increases as navigators try to get support from family or friends. So a key part of putting a patient navigation program in place is establishing support structures for the navigators.
"Inherent in the navigator's function is caring for the emotional health of patients," he said. "Navigators need to have resources and methods that will allow them to cope with the inevitable stress of the burden-sharing process. What works in this arena depends on the individual, but methods of support must be recognized and facilitated by administration as a normal part of the navigator's job description."