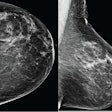
Back in the day, screening for breast cancer mostly consisted of a mammography exam. But with increased understanding of risk factors such as breast density and the advent of new technologies, breast cancer screening isn't a one-size-fits-all endeavor anymore, according to a presentation at the AHRA 2016 meeting in Nashville, TN.
Determining how to offer multimodality, personalized screening can be tricky, in part because it's often unclear which modality is best as a mammography adjunct, said presenter Gerald Kolb, president of the Breast Group in Bend, OR, and consultant to breast imaging software developer Volpara Solutions.
"Individualized screening is based on using risk assessment [with] tools like the Tyrer-Cuzick model to assess family history, and evaluating density," he said. "But there are challenges, such as operator variability in breast density assessment and [the question of] which supplemental modality to use."
Why individualize?
Why should breast cancer screening be individualized? Because mammography misses some cancers, particularly in women with dense breast tissue, according to Kolb.
"The goal of screening is to positively impact outcomes, reducing mortality and morbidity as well as the cost of treating later-stage cancers," he said.
Individualized screening is generally defined as multimodality screening individually applied to women based on their relative risk. The American Cancer Society recommends that women with a 20% to 25% lifetime risk of breast cancer undergo breast MR. Women at increased risk (15% to 20%) should have mammography plus supplemental ultrasound, while women at normal risk can stick with mammography alone, Kolb said.
A woman's breast cancer risk can be assessed using her tissue density and tools like the Tyrer-Cuzick model. But there are challenges to risk assessment, including operator variability in evaluating density -- which some facilities address with automated density assessment software -- and fitting multimodality screening into a facility's workflow, according to Kolb.
So what supplemental modality should you choose? Automated ultrasound is a good place to start, he said. MRI and molecular imaging require the injection of contrast or isotopes; MR requires precertification and only women at high risk qualify for it. But automated ultrasound can easily accommodate the timing and volumes expected in a multimodality screening program.
"Additional screening must be convenient: Patients are busy, and some studies have found only a 30% compliance rate if they need to come back for supplemental imaging," Kolb said.
Density education
Along with offering a multimodality screening program, facilities need to educate patients about breast tissue density, according to Kolb. One way to do this is to send them a brochure along with their exam reminder letter that explains density and how it may limit the sensitivity of mammography. And when the patient appears for her exam, a chat with the technologist also helps.
"Most patients never have contact with the radiologist who reads their mammogram," he said. "The technologist tends to be the most visible person in the screening process."
It's also crucial to educate referring physicians about the benefits of early breast cancer detection, perhaps through a personal letter that includes information about breast density -- or face-to-face contact with the department's top 10 referrers.
"Primary care physicians generally welcome radiology taking the lead with their patients in regards to breast imaging," Kolb said.
Go with the flow
Once you've created a multimodality screening program, make sure to market its benefits to the women in your community, Kolb said.
"Imaging surveillance is still the only way to achieve early detection of breast cancer," he said. "And early detection offers the best prognosis for recovery."
The bottom line is that new screening challenges will arise and different technologies will make their way into clinical practice. But the mission remains the same.
"Our goal is to reduce the impact of breast cancer on the populations we serve, through early detection achieved by providing excellent clinical care," Kolb concluded. "Keep your focus on solutions, not the problems."