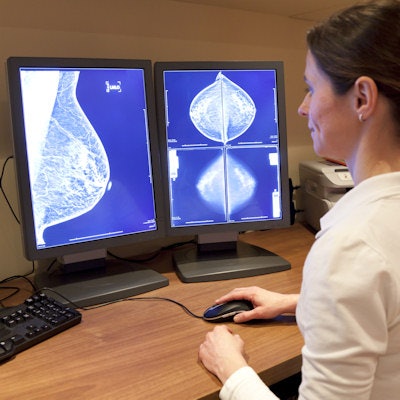
A few simple interventions can significantly reduce recall rates for both full-field digital mammography (FFDM) and digital breast tomosynthesis (DBT), according to a study published online July 28 in Academic Radiology. And the interventions don't add much more time to a busy practice's workload, researchers found.
Since reducing recalls is a key component of mitigating mammography's "harms," the study findings are good news not only for women but also for breast imagers who are interested in providing the most efficient patient care, wrote a team led by Dr. Lisa Mullen from Johns Hopkins University in Baltimore.
"Decreasing recall rates while maintaining critical quality metrics enhances value and improves patient-centered care," the group wrote. "Simultaneously, this approach saves healthcare expenses, time, and resources while decreasing 'false alarms' and the resultant distress for women."
Recall reduction
Screening mammography helps find cancers earlier, but it can also produce results that prompt a woman to be called back for further assessment, with more imaging and/or a biopsy. These recalls can be upsetting for patients -- and expensive, Mullen's group noted.
"False-positive screening recalls and the resulting additional evaluation may cause significant psychological distress to women," the authors wrote. "There are significant financial costs associated with false-positive recalls in the United States. One report suggests an annual cost of $1.6 billion in the United States for recall utilization resulting from mammographic screening."
Mullen and colleagues sought to evaluate how two different interventions might influence the performance metrics of 10 breast imagers, such as recall rates, cancer detection rates, and positive predictive value for recall (PPV1). The group gathered FFDM and DBT baseline data for a three-year period (January 2012 to February 2015) before the two interventions, then evaluated mammography performance metrics after each.
The two interventions were as follows:
- An "awareness" intervention: Researchers conducted an educational effort to increase awareness among breast imagers of recalls from screening mammography. This included discussion regarding screening recalls and radiologist review of their recalled cases, and it was conducted from February 2015 to September 2015
- A "consensus" intervention: This consisted of consensus double reading of all recalls and was conducted from September 2015 to April 2016.
For the awareness intervention, radiologists reviewed 4,296 FFDM and 7,287 DBT exams; for the consensus intervention, radiologists reviewed 2,900 FFDM and 9,190 DBT exams.
The awareness intervention produced a statistically significant decrease in recall rate for FFDM and DBT compared with the baseline period (p = 0.0001 and p = 0.018, respectively), and a statistically significant increase in the PPV1 rate for DBT compared with baseline (p = 0.0001). The consensus intervention produced a statistically significant decrease in recall rate for FFDM compared with baseline (p = 0.048) and also a statistically significant increase in the PPV1 rate for both FFDM and DBT compared with baseline (for both, p = 0 .0001).
| Impact of interventions on mammography screening metrics | ||||||
| Baseline | Awareness intervention | Consensus intervention | ||||
| FFDM | DBT | FFDM | DBT | FFDM | DBT | |
| Recall rate | 11.1% | 7.6% | 9.2% | 6.6% | 9.9% | 7.2% |
| Cancer detection rate (per 1,000) | 3.8 | 4.8 | 3.1 | 6.2 | 5.9 | 5.7 |
| PPV1 | 3.4% | 6% | 3.1% | 10.8% | 5.7% | 9% |
"The effect of outcome awareness and consensus recall appeared greater with FFDM compared to DBT, likely due to the already reduced recall rates associated with the 3D technique," Mullen and colleagues wrote. "This may also be related to less confidence about findings on FFDM, and therefore more opportunity for improvement and better outcomes with two readers."
Overall trends of decreased recall and increased PPV1 rates were generally distributed across all age groups, according to the researchers.
Finally, they found that each recall consultation for the consensus intervention took an average of 2.3 minutes.
"Our study demonstrates that double reading only potential recalls was efficient, with an average of 2.3 minutes spent on each case," they wrote. "One must also consider the breast imager's time that is recovered by avoiding diagnostic workups that result from false-positive screening recalls."
Which is better?
Which intervention is best? It depends on a practice's goals and available time to allocate measures such as these, according to the authors. The consensus intervention increased PPV1 rates for both screening modalities, demonstrating that more patients were recalled appropriately. But the awareness intervention, in which breast imagers reviewed their own recalls, resulted in a more dramatic recall rate reduction.
"Interestingly, the reduction in recall rate attributed to review of personal recalls was actually more substantial than the reduction attributed to consensus double reading, for both FFDM and DBT," the team wrote. "This unexpected result suggests that the motivated radiologist could invest a small amount of time each week reviewing his or her own recalls, and thereby improve his or her personal performance metrics."
In any case, study's findings suggest that simple interventions such as these can decrease recall rates and also lead to more efficient workflow, reduced healthcare costs, and less patient stress, the authors concluded.
"Using review of one's own screening recalls as well as requiring consensus of two readers for potential recalls can safely decrease recall rates," the team wrote. "We ... propose that these interventions can be implemented and scaled to both community and academic settings to improve performance."