One-view digital breast tomosynthesis (DBT) detects 34% more breast cancers than traditional mammography -- with a majority of the detected tumors proving to be invasive cancers, according to a large clinical study in Sweden.
The study included almost 15,000 women screened over a period of five years who first underwent two-view digital mammography screening and then one-view DBT with reduced compression during another visit. DBT demonstrated a higher sensitivity at 81.1% versus 60.4% for digital mammography, according to lead author Dr. Sophia Zackrisson, an associate professor at Lund University and a radiologist at Skåne University Hospital in Malmö.
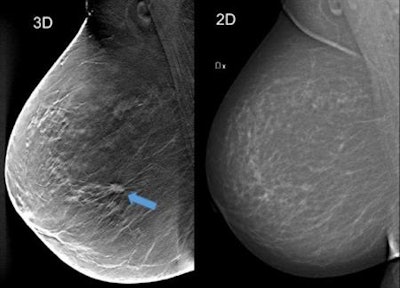 Using breast tomosynthesis (3D screening) in the image to the left (one of about 50 thin cross-sectional image slices of the breast), you can see an approximately 1 cm-large tumour that is not clearly visible on the mammography image on the right, even though the breast does not contain particularly dense tissue. Image courtesy of Skåne University Hospital in Malmö.
Using breast tomosynthesis (3D screening) in the image to the left (one of about 50 thin cross-sectional image slices of the breast), you can see an approximately 1 cm-large tumour that is not clearly visible on the mammography image on the right, even though the breast does not contain particularly dense tissue. Image courtesy of Skåne University Hospital in Malmö."If supported by cost-effectiveness studies, one-view digital breast tomosynthesis warrants consideration as the preferred breast cancer screening method in the future," she and her colleagues wrote (Lancet Oncology, October 12, 2018).
DBT vs. mammography
DBT is emerging as an improved breast cancer screening method, with previous studies showing increased cancer detection compared with traditional mammography. Two-view DBT combined with synthesized digital mammography, which uses 2D images reconstructed from the DBT image dataset, has shown promising results in prospective trials and overcomes the problem of increased radiation exposure associated with combining DBT and digital mammography.
To further simplify breast cancer screening using DBT, the prospective, population-based Malmö Breast Tomosynthesis Screening Trial (MBTST) investigated single-view DBT (mediolateral oblique [MLO] view) compared with conventional two-view digital mammography.
"This strategy minimizes the radiation dose to women undergoing breast cancer screening and reduces the extent of screen-reading compared with dual-imaging methods," Zackrisson and colleagues wrote.
They enrolled 14,851 women from January 2010 to February 2015 at Skåne University Hospital. Women ages 40 to 74 were randomly selected to receive two-view digital mammography (Mammomat Inspiration, Siemens Healthcare) followed by one-view DBT (also Mammomat Inspiration). To reduce discomfort for the women during examination, the screening trial used reduced compression force for DBT.
They found DBT detected more cancers but had lower specificity and a higher recall rate. Results are summarized in the table below.
| One-view DBT vs. mammography in Sweden | ||
| Digital mammography | One-view DBT | |
| Sensitivity | 60.4% | 81.1% |
| Specificity | 98.1% | 97.2% |
| Recall rate | 2.5% | 3.6% |
| Positive predictive value | 25.9% | 24.1% |
| Negative predictive value | 99.6% | 99.8% |
| Mean glandular radiation dose | 2.7 mGy | 2.3 mGy |
The mean compression force in the MLO projection was 118 Newtons (N) at digital mammography and 71 N at DBT -- a mean reduction of 40% in the compression force.
"By not compressing too much you actually achieve more image slices of the breast and hence increased depth resolution," Zackrisson told AuntMinnie.com. "The effect on radiation dose is minor because the breast thickness does not increase much and we still used on average 15% lower dose with one-view DBT compared with two-view digital mammography."
The researchers didn't use synthesized 2D DBT, and their findings indicate the possibility of a more streamlined screen-reading process with a lower image-reading burden for standalone one-view DBT compared with the more common two-view DBT with synthesized mammography.
"All cancers except two found by the digital breast tomosynthesis reading group were detected in the first reading step -- i.e., one-view digital breast tomosynthesis only," the study authors wrote. "Thus, the increase in cancer detection by including the craniocaudal view of digital mammography with digital breast tomosynthesis was small."
Before introducing DBT in the general breast cancer screening program, Zackrisson and colleagues are conducting a cost-benefit analysis. They are also conducting a metastudy with European colleagues in which they will aggregate and analyze their collective research results.
An analysis of interval cancers in the trial will be compared with a large contemporary screening cohort, which the authors will present at RSNA 2018, Zackrisson wrote in an email.
In the future, parts of the image review in connection with DBT may be automated with the help of computers, but it will take time. There is currently a lack of appropriate ready-to-use and tested software, but studies are underway, including in Zackrisson's research team.
"We are interested in moving forward with individualized, risk-based screening as well," she wrote. "DBT is a great start, but there are women whose cancers are not visible with DBT either. I think some of our future trials will focus on that."
Study disclosures
Dr. Sophia Zackrisson and several co-authors received funding for traveling and speaker's fees from Siemens Healthcare. She and some of her colleagues also have a patent (U.S. Patent No. 9,833,203) issued for a compression device for x-ray and mechanical imaging of a breast.