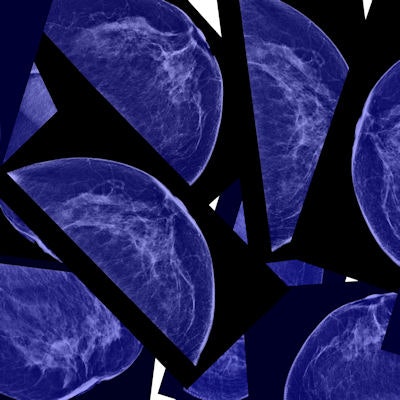
Women may be almost 60% less likely to be assigned to a dense breast category if they are evaluated with 3D digital breast tomosynthesis (DBT) compared with standard digital mammography, according to a new study published online March 19 in Radiology.
The findings could affect clinical decisions about supplemental breast screening and risk assessment, wrote a team led by Aimilia Gastounioti, PhD, of the University of Pennsylvania.
 Aimilia Gastounioti, PhD, of the University of Pennsylvania.
Aimilia Gastounioti, PhD, of the University of Pennsylvania."Our hypothesis is that these different mammographic screening modalities may result in a different perception of density, reflected in a different assignment of BI-RADS density categories," the group wrote.
But the implications of density downgrades could be mixed, wrote Dr. Liane Philpotts of Yale University, who wrote an accompanying editorial but was not involved in the study.
"Because density is a major limitation of mammography, this visual lessening of density could be a good thing," she wrote. "If, in fact, it proves artificial, then it could be detrimental, potentially resulting in some cancers going undetected."
Density matters
Women with high levels of breast tissue density have four to six times the risk for breast cancer compared with women with low density, the group wrote. Density is most commonly measured using the American College of Radiology's (ACR) BI-RADS system, which includes four categories of breast density:
- Almost entirely fatty
- Scattered areas of fibroglandular density
- Heterogeneously dense
- Extremely dense
More than 70% of U.S. states have legislation that requires healthcare providers to inform women of their breast density and their options for supplemental breast cancer screening since 2D mammography's sensitivity is compromised in dense breast tissue.
But what if using 3D mammography could downgrade some women's density category -- and perhaps reduce the cost and inconvenience of supplemental imaging? To address this question, Gastounioti's team investigated the effect of screening modality on BI-RADS density assessments.
The study included data from 24,736 women who underwent mammography screening at the Hospital of the University of Pennsylvania between 2010 and 2017. The researchers noted each woman's breast density category, race, age, and body mass index (BMI); the study population was 46% white and 54% African-American.
Of 60,766 imaging exams, 8,935 were performed with digital mammography (14.7%), 30,799 with digital mammography plus DBT (50.7%), and 21,052 with synthesized 2D mammography and DBT (34.6%).
Gastounioti's group found the following:
- Compared with digital mammography alone, women who were imaged with digital mammography combined with DBT were 31% less likely to be categorized as having dense breast tissue.
- Those imaged with synthesized 2D mammography and DBT were 57% less likely.
- A woman's odds of being categorized as having high breast tissue density was reduced by 38% when synthesized 2D mammography was used instead of conventional 2D mammography.
"Our findings showed an overall trend of downgraded breast density when imaging was performed with either digital mammography plus DBT or synthetic 2D mammography plus DBT, compared with digital mammography alone," Gastounioti told AuntMinnie.com. "The density downgrade may be due to the perception of less fibroglandular tissue in the 3D display of DBT imaging compared with digital mammography's flat, 2D display, as well as differences in the appearance of the denser glandular tissue and the more lucent, fatty tissue in the reconstructed synthetic 2D imaging."
Finally, the researchers discovered that changes in breast density categories due to different screening modalities were greater for black women than for white women and for women with higher BMI measures.
"Breast density levels appear to vary by modality, race, and BMI," she said. "Such variations may affect the number of women offered supplemental screening and, potentially, risk assessment. There seems to be a need to adjust breast cancer screening guidelines by [these factors]."
Clinical implications
The results of this study must be considered carefully, according to Philpotts. If fewer women are categorized as having dense tissue using 3D mammography, then fewer may be recommended for supplemental imaging -- which could mean some cancers are missed.
"If more women are classified as having nondense breast tissue, they will not be eligible for supplemental screening," she wrote. "Such screening, particularly with ultrasound or MRI, has been shown to detect occult cancers at mammography. Downgrading of density could result in some of these cancers going undetected."
In any case, it's clear that breast tissue density categories need to be refined, Philpotts noted.
"One definite take-home lesson is that more rigorous and sophisticated imaging categorization of density is needed that will hopefully result in more uniform density designation between modalities and vendors, and more relevance to breast cancer risk and tailored screening guidelines," she concluded.