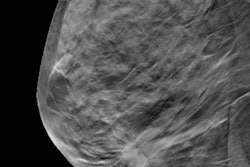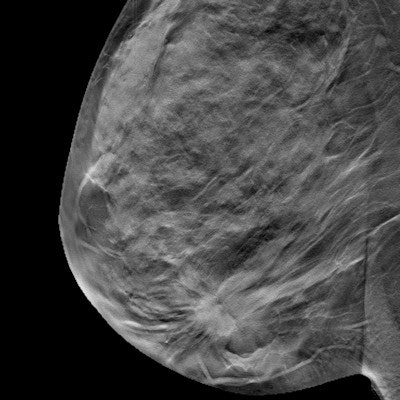
Digital breast tomosynthesis (DBT) had significantly lower recall rates than digital mammography in a study published on March 30 in JAMA Network Open. The modality also had higher rates of breast cancer detection, suggesting the reduction in recalls wasn't because of missed cancer cases.
The large, U.S.-based study included more than 2 million breast screening examinations read by 198 radiologists. The recall rate for DBT also stayed lower than digital mammography even after researchers adjusted for outside trends and confounding factors.
"Our results demonstrate a clinically important downward shift in the distribution of radiologist recall rates with DBT screening among a large, geographically diverse sample of U.S. radiologists," wrote the authors, led by Brian Sprague, PhD, from the University of Vermont Cancer Center.
The American College of Radiology recommends a mammography recall rate of no more than 12%, according to the authors. However, some surveys have found that fewer than two-thirds of radiologists actually fall below this threshold. The authors wondered whether the increase in DBT screening may have improved that statistic.
For their study, they used data from six Breast Cancer Surveillance Consortium registries, covering a cohort of U.S. radiologists from various practice settings. The authors looked at the radiologists' recall and cancer detection rates before and after they began using DBT. They also included some radiologists who only read digital mammography results to adjust for other trends.
The mammography recall rate fell from 10% before DBT use to 8.8% after the addition of DBT. Further, the number of radiologists staying within the 12% recall rate threshold rose from 66% before DBT implementation to 76% after DBT use.
Importantly, the recall rate with DBT stayed significantly lower than digital mammography after the authors adjusted for confounding variables and outside trends. After adjustment, recall rates were 15% lower on DBT examinations.
Radiologists who interpreted DBT examinations also found significantly more cancers after the switch to DBT. The authors found a cancer detection rate of 4.7 per 1,000 examinations before DBT use. That number rose to 5.3 per 1,000 examinations in the DBT era.
The recall rates didn't improve evenly for all radiologists in the study, though. Half of the radiologists in the study had no difference in recall rates after the addition of DBT. Another 14% saw an increase in patient recalls.
"Radiology practices should audit radiologist DBT performance statistics closely and consider additional DBT training for radiologists whose screening performance does not improve as expected," the authors concluded. "Policymakers and women should be informed that most women undergoing DBT examinations will experience a reduced recall rate and elevated cancer detection rate, although these benefits will vary substantially depending on the individual radiologist interpreting the examination."