Missed cancers on breast imaging can be deadly for patients and costly for radiologists. But acknowledging the existence of six cognitive biases may help prevent missing a crucial breast cancer diagnosis, according to a June 12 article in Radiographics.
Cognitive biases are a natural part of human cognition and are the result of deriving information from subjective sources as opposed to present, objective truth. Such biases can lead to critical thinking or judgment errors.
When it comes to breast cancer, these cognitive biases can result in overreliance on previous findings and experiences. In particular, they can lead to missing cancers that are slow-growing, are characteristic of benign lesions, or have subtle features of malignancy.
"To minimize cognitive bias, radiologists should continuously question themselves and evaluate their thought processes," wrote the authors, led by Dr. Leslie Lamb, a breast imaging radiologist at the University of Ottawa's Ottawa Hospital.
Commonly missed breast cancers often share some similarities. They may appear stable on more recent mammograms but are actually slowly changing over time. They may also get classified as "probably benign" findings or can result from radiologists not taking the time to carefully evaluate calcifications and architectural distortions.
While not every missed breast cancer is the result of human error, cognitive biases play a role in missing breast cancers that are present on imaging exams. The authors noted that six types of cognitive biases are particularly important for breast imaging.
1. Satisfaction-of-search bias
Satisfaction-of-search bias is a decreased awareness of vigilance when finding a second abnormality after the first has been identified. This bias is particularly common in diagnostic radiology, the authors noted.
For breast imaging, it is not uncommon for multiple breast cancers to appear in the same quadrant or different quadrants. Therefore, to overcome this bias, it is crucial for radiologists to continue searching for additional disease sites after discovering a first.
2. Inattentional blindness bias
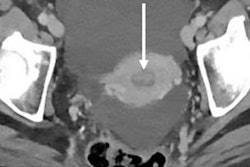
Inattentional blindness bias is akin to experiencing "tunnel vision" and missing something "hiding in plain sight." For expert radiologists, this bias could result in not checking seemingly irrelevant areas, since their mind has been trained by experience to look for findings in more clinically significant areas.
To overcome inattentional blindness, radiologists should be aware of blind spots and take time to look at the full view of the breast. This can help spot cancers that appear as large or diffuse abnormalities.
3. Hindsight bias
Hindsight bias is de-emphasizing the difficulty of a decision in retrospect. Breast cancer is difficult to diagnose, and sometimes failing to identify cancer on imaging does not necessarily mean radiologic error, the authors noted.
When reviewing previous cases, it is important to ask, "What can I learn from this case?" as opposed to more pointed questions, such as "How could I have missed that?" It is also important to not let retrospective analysis result in under- or overconfidence.
4. Anchoring bias
Anchoring bias is relying too much on early findings to make subsequent decisions. For radiologists, this often means not adjusting a diagnosis to new, relevant information.
To avoid anchoring bias, radiologists should not form a diagnosis before viewing all relevant information. They should also try to disprove an initial hypothesis, the authors noted.
5. Premature closing bias
Premature closing bias is coming to a conclusion without a full and complete investigation, and it is one of the most common biases in medicine.
In radiology, premature closing bias may present as classifying a lesion as benign or probably benign finding, even if it does not strictly meet that categorization. It can also result in not adequately following up on negative biopsies to ensure the results were not a false negative.
6. Satisfaction-of-reporting bias
Satisfaction-of-reporting bias is being influenced by another person's interpretation. To overcome this bias, radiologists should review findings and generate their own impression before reading a prior report. Radiologists can also consider getting a second opinion for equivocal cases.
The above biases can contribute to missed breast cancer cases, but the good news is that radiologists can take steps to improve their screening effectiveness. For instance, breast imaging training, peer review, and self-audits can all help reduce missed cancers.
"In summary, always remember to finish a case by asking at least one question, such as Did I check my blind spots?" the authors concluded. "The short amount of time that it takes to ask that extra question ... may aid in averting a missed breast cancer."