A woman's race/ethnicity and her education and income levels affect her likelihood of having access to digital breast tomosynthesis (DBT) for breast cancer screening, according to a study published February 19 in JAMA Network Open.
These findings persist even though more women's health facilities have incorporated DBT into their breast cancer screening arsenal, wrote a team led by Dr. Christoph Lee of the University of Washington in Seattle.
"Even as onsite access to DBT improved over time, our analysis demonstrates disparities in DBT use based on socioeconomic characteristics," Lee and colleagues noted.
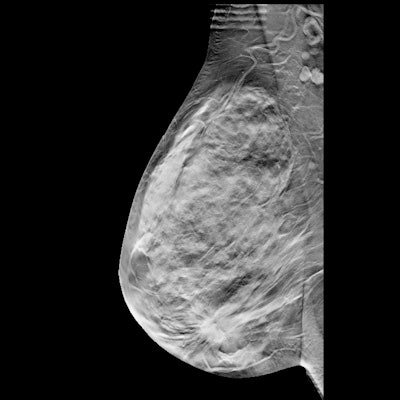
Although DBT has been lauded for its ability to reduce recalls and find cancers that are often hidden on conventional digital mammography, it isn't clear whether all women have equal access to the technology, the researchers wrote. To further complicate the issue of access, not all breast care facilities are able to purchase and offer DBT, and insurance coverage for the technology varies.
"Populations with traditional disparities -- Black race, Hispanic ethnicity, lower educational level, or lower income level -- have historically experienced greater breast cancer morbidity and mortality than their less disadvantaged counterparts," they wrote. "These populations have also historically been the last to benefit from newer medical technologies."
Lee's group assessed women's DBT access and determined whether factors such as race and ethnicity, educational level, or income influenced this access using information from 92 imaging facilities in five U.S. states. The data included 2.3 million screening DBT exams performed in women 40 to 89 years of age between January 2011 and December 2017.
The authors found that overall access to DBT increased dramatically during the study timeframe, from 3.3% in 2011 to 82.6% in 2017. But race/ethnicity and education and income levels influenced women's access, with women of color, those with less education, and those with less income having less access to DBT screening.
| Access and use of DBT for breast cancer screening by sociodemographic factors | ||
| Characteristic | DBT available at screening | DBT used if available at screening |
| Race/ethnicity | ||
| Asian | 16.5% | 42.8% |
| Black | 34.4% | 37.7% |
| Hispanic | 30.6% | 44% |
| White | 37.2% | 53.1% |
| Educational level | ||
| Less than high school diploma | 16.4% | 40.8% |
| High school diploma | 25.7% | 47.7% |
| College degree | 25.5% | 50.6% |
| Income quartile | ||
| Low (less than $60,781 per year) | 31.8% | 43.9% |
| Medium ($77,664 to $93,952) | 32.7% | 52.4% |
| High (greater than $93,952) | 28.8% | 51.4% |
Insurance coverage is also an access factor, the team noted.
"Medicare did not reimburse for DBT until 2015, and third-party payer coverage for DBT remains payer dependent, which suggests that insurance coverage and copayments may be an important factor for trends in DBT use," it wrote.
Clearly, interventions are needed to address the disparity of access to DBT, according to Lee and colleagues.
"Radiology practices and policy makers should be cognizant of these screening access and use differences, and future efforts should address racial/ethnic, educational, financial, and geographic barriers to obtaining DBT screening at the facility level," they concluded.
Uptake discrepancies
In a related study published February 16 in the Journal of the American College of Radiology, a team led by Dr. Nila Alsheik of Advocate Caldwell Breast Center in Park Ridge, IL, used data from 63 U.S. breast imaging centers that included 385,503 women who underwent 542,945 DBT and 261,359 digital mammography exams.
These researchers found that, despite DBT's improved performance over digital mammography alone, fewer Black women underwent DBT screening compared with their white or Asian counterparts, at 44% versus 61% and 63%, respectively.
"All racial groups had improved outcomes with DBT screening, but disparities were observed in DBT utilization," Alsheik and colleagues concluded. "These data suggest that reducing inequities in DBT utilization may improve the effectiveness of breast cancer screening."
Disclosure: Alsheik is a scientific advisory board member for Hologic and has received research support from the firm.




















