It's no secret that radiologists' interpretive accuracy on screening mammography can vary widely. But the particular factors that influence performance may come as a surprise, according to a study published June 22 in Radiology.
A team led by Dr. Cindy Lee of NYU Langone Health in New York City found that characteristics beyond a radiologist's time in practice, for example, can affect mammography interpretation performance.
"The geographic location of the radiology practice, subspecialization in breast imaging, and performance of diagnostic mammography are associated with better screening mammography [interpretations]," the authors wrote.
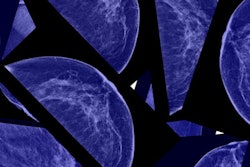
Previous research on radiologists' mammography interpretation accuracy has focused on individuals' clinical experience and have relied on subjective surveys, Lee's group noted. Other factors, like demographic characteristics or clinical practice patterns, aren't as well understood. To address the knowledge gap, Lee's group conducted a study that included data from 1,223 radiologists from the National Mammography Database between 2008 and 2019. The team tracked radiologists' demographics, subspecialization, and clinical practice patterns, and then used the following seven metrics to assess mammography interpretation performance:
- Recall rate between 5% and 12%
- Cancer detection rate of at least 2.5 per 1,000 screening exams
- Positive predictive value of recall (PPV1) between 3% and 8%
- Positive predictive value of biopsies recommended (PPV2) between 20% and 40%
- Positive predictive value of biopsies performed (PPV3) between 25th and 75th percentile of the study sample
- Invasive cancer detection rate of at least the 25th percentile of the study sample
- Percentage of ductal carcinoma in situ (DCIS) of at least the 25th percentile of the study sample
Lee and colleagues found that geography played a part in mammography interpretation accuracy, with Midwestern radiologists more likely to have higher performance in recall rate, PPV1, PPV2, and cancer detection rate than their Northeast counterparts (odds ratio, 1.4), and Western radiologists performing better than their peers in recall rate, PPV2, and PPV3 (odds ratio, 1.7).
Specialization helped as well, with breast imagers more likely to reach acceptable PPV1, invasive cancer detection, percentage DCIS, and overall cancer detection compared with general radiologists (odds ratio, 1.4). Radiologists who read diagnostic mammography exams also performed higher than those who did not in the following measures: PPV1, PPV2, PPV3, invasive cancer detection, and overall cancer detection (odds ratio, 1.9).
The study results not only confirm that there are variations among radiologists when it comes to breast cancer screening interpretation but also the importance of training, according to the authors.
"[Our] findings indicate not only variation in radiologist performance in screening mammography nationally but also the association of such variation with specific radiologist characteristics in a predictable manner that can be applied to predict those radiologists with better or worse performance," they concluded. "Furthermore, the findings support the value of breast subspecialization in achieving better patient outcomes among radiologists who interpret screening mammography."