The time is now to take steps toward removing barriers and promoting inclusion in breast cancer screening for transgender people, according to an editorial published online June 22 in Academic Radiology.
Researchers led by Dr. Faheemullah Khan from Aga Khan University Hospital in Pakistan authored the editorial, which outlined current scientific knowledge of trans people in breast cancer screening, as well as socioeconomic barriers preventing more widespread screening in this community. They also detailed specific concerns about trans breast cancer screening in Pakistan.
"The pervasive stigma about the transgender community is deeply rooted around the globe in all spheres of public life," Khan et al wrote. "Health, as a fundamental human right, was enshrined in the Universal Declaration of Human Rights in 1948, Article 25. However, even after more than 70 years, communities such as transgenders face the worst form of discrimination while seeking healthcare."
Less than 1% of the U.S. identifies as being trans, though researchers have pointed out that this may be an underestimate due to social stigmas. A majority of trans women use gender-affirming hormones, which were found in a 2019 study to increase breast cancer risk by 43 per 100,000 person-years. The same study also found that trans women have 46 times higher breast cancer risk than cisgender men and that breast cancer follows a rapid course after a latent period of 18 years of hormone use.
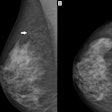
Current guidelines suggest that trans people who have used gender-affirming hormones for over five years should receive mammograms every other year. However, screening is not advised for trans people over 50 years old, unless they have a history of gender-affirming hormone use. Previous research has shown that screening before 50 has no proven benefit.
Guidelines also suggest that oncologic follow-up is needed if BRCA mutations are found in trans women using gender-affirming hormones. Known cases of BRCA mutation or with a family history of breast cancer require genetic counseling and screening.
Previous research suggests that trans men who have not undergone bilateral mastectomy or who have only undergone breast reduction should still have screening done.
The editorial authors wrote that raising awareness among both clinicians and trans patients is more important than initiating screening at a younger age or enhancing available screening. Studies have shown that trans patients are less likely to seek breast cancer screening than their cisgender counterparts.
They also wrote that mammograms have "never" been performed on trans women in Pakistan, based on administrative information from major Pakistani hospitals.
"This represents the lack of uniformity in the health care setting, resulting in an increase in undiagnosed occurrences of breast cancer among transgenders," they added.
The authors added that culturally sensitive healthcare tailored to trans people is "vital" and gave examples such as the World Health Organization (WHO) supporting incorporating trans health into the standard medical curriculum. A 2022 study the team cited found that healthcare education systems using audits can help drive LGBTQIA+ inclusion and participation in academic settings.
They emphasized that breast cancer is a serious concern in trans people.
"In countries such as Pakistan, health care is on the brink, therefore, caring for transgenders would require revolutionary measures," the authors wrote. "It is high time that important steps for breast cancer screening in transgenders are considered."