Digital breast tomosynthesis (DBT) shows improved screening mammography outcomes over those seen in digital mammography, according to a study of over 1 million women published March 14 in Radiology.
Researchers led by Dr. Emily Conant from the University of Pennsylvania in Philadelphia found that DBT had lower recall rates and higher cancer detection rates in women compared with digital mammography.
"This study further substantiates that digital breast tomosynthesis should be the standard of care for mammographic screening," Conant told AuntMinnie.com.
Previous research suggests that DBT in screening mammography settings has the potential to replace digital mammography, owing to lower recalls and more breast cancers detected.
However, Conant's team noted that many studies evaluating DBT's benefits over digital mammography have been conducted with a focus on specific areas, such as imaging dense breast tissue or detecting interval or advanced cancers. Conant and colleagues sought to explore screening outcomes in a large cohort of U.S. women who underwent routine digital mammography or DBT mammographic screening.
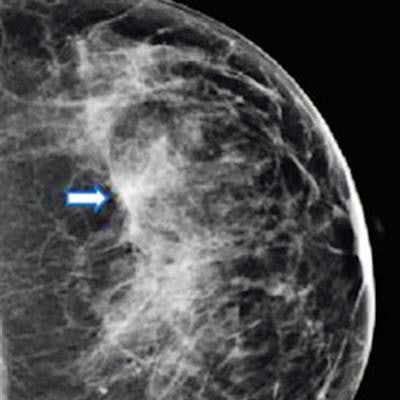
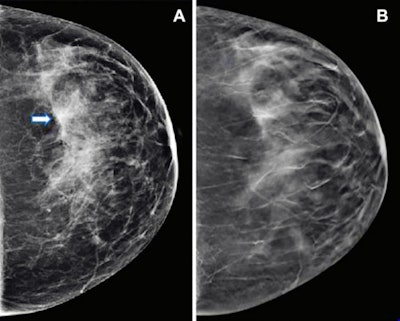 Images show mammography results in a 47-year-old woman who presented for routine screening. (A) Craniocaudal digital mammogram shows scattered fibroglandular densities. On the left digital mammographic craniocaudal view laterally, an asymmetry (arrow) is present. (B) Left craniocaudal DBT imaging shows no suspicious lesion, but rather a superimposition of normal fibroglandular and ligamentous structures. Images and caption courtesy of the RSNA.
Images show mammography results in a 47-year-old woman who presented for routine screening. (A) Craniocaudal digital mammogram shows scattered fibroglandular densities. On the left digital mammographic craniocaudal view laterally, an asymmetry (arrow) is present. (B) Left craniocaudal DBT imaging shows no suspicious lesion, but rather a superimposition of normal fibroglandular and ligamentous structures. Images and caption courtesy of the RSNA.They evaluated data from 2.5 million screening mammograms from 1.1 million women between the ages of 40 and 79. The women had no prior history of breast cancer and were screened from 2014 to 2020 in five U.S. healthcare systems. The researchers collected information from 1.7 million screening DBT exams and 834,336 screening mammograms from digital mammography.
They found a significant increase in cancer detection, reduction in recall, and positive predictive value of recall (PPV1) for DBT when compared with digital mammography.
| Outcomes for DBT vs. digital mammograhy | |||
| Measure | Digital mammography | DBT | p-value |
| Recall rate | 10.3% | 8.9% | < 0.001 |
| Cancer detection rate (per 1,000) | 4.5 | 5.3 | < 0.001 |
| PPV1 | 4.3% | 5.9% | < 0.001 |
| Biopsy rates (per 1,000) | 14.5 | 17.6 | < 0.001 |
The group also found that the positive predictive value for biopsy (PPV3) was similar between both modalities, at 29.3% for DBT and 30% for digital mammography. When the team adjusted for age, breast density, site, and baseline screening year, it found no statistically significant differences.
These results confirm what other studies examining DBT's potential benefits have shown, "but on a much larger scale," Conant said, adding that this further validates the improved screening outcomes associated with DBT. She and her colleagues noted that the study results could be used in future analyses that require large data sets.
"Next steps will be further investigation of subgroups of patients in this large dataset, as well as the monitoring of longer-term outcomes such as breast cancer morbidity and mortality," Conant told AuntMinnie.com.
Disclosure: Conant receives grants and consulting fees from iCAD; consulting fees from Hologic; and payment for lectures for Hologic, MedScape, and AuntMinnie.com.