Implementing AI-based computer-aided detection (CAD) software can improve the performance of radiologists interpreting automated breast ultrasound (ABUS) exams, suggest findings published October 7 in Academic Radiology.
Researchers led by Mi-ri Kwon from Kangbuk Samsung Hospital in Seoul in South Korea also found that cancers detected by AI-CAD were smaller, less frequently showed retraction phenomenon, and had lower BI-RADS categories.
“As a second reading or concurrent double-reading tool, it (AI-CAD) can help avoid the oversight errors that may occur with ABUS,” Kwon and co-authors wrote.
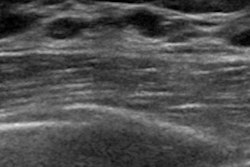
Previous studies suggest that ABUS has advantages over conventional breast ultrasound, including providing high-resolution 3D images with multiplanar reformations and reducing operator dependence by increasing consistency and reproducibility. However, the researchers pointed out that ABUS still has its share of disadvantages. These include generating volumetric image data with many slices, which can cause oversight errors. It also has limited ability to assess the axilla, vascularity, and elasticity of lesions.
The Kwon team sought to test the performance of an AI-CAD system that automatically scans 3D volume images. It detected suspicious areas and visualized only the results with a high likelihood of malignancy, using commercially available CAD software (LuCAS-ABS, Monitor Corporation).
For the study, the researchers included data from 262 ABUS-detected breast lesions in 231 women taken between 2020 and 2022. Of the total, 145 lesions were malignant, while 117 were benign. From there, two radiologists reviewed the images and assigned a BI-RADS category, and the AI-CAD system classified them as positive or negative.
The team determined the AI-CAD-aided BI-RADS categories in four ways. First, the radiologists checked the results and decided whether to modify the BI-RADS category (AI-aided 1). Second, the BI-RADS category was upgraded or downgraded based on the AI-CAD results (AI-aided 2). Third, the BI-RADS category was upgraded only when the AI-CAD results were positive (AI-aided 3). Fourth, the category was downgraded only when the AI-CAD results were negative (AI-aided 4).
The researchers found that compared with the radiologists only, the AI-CAD system significantly improved the overall diagnostic performance, represented by area under the curve (AUC) values.
| Performance of radiologists, AI-CAD software on ABUS |
||
|---|---|---|
| |
AUC |
p-value |
| Radiologists |
0.87 |
N/A (reference) |
| AI-aided 1 |
0.919 |
0.001 |
| AI-aided 2 |
0.884 |
> 0.99 |
| AI-aided 3 |
0.89 |
0.41 |
| AI-aided 4 |
0.89 |
0.43 |
The researchers also found that among nonmass lesions, AI-CAD-negative cancers showed no posterior shadowing. Also, AI-CAD-negative cancers were smaller (1.0 cm) compared to positive cancers (2.1 cm, p < 0.001).
For masses, most AI-CAD-negative cancers showed no retraction phenomenon compared to AI-CAD-positive cancers (86.4% vs. 41.6%, p < 0.001). Among nonmass lesions, 60% of AI-CAD-positive cancers had posterior shadowing, while all AI-CAD-negative cancers showed no posterior shadowing (p = 0.02).
Finally, the researchers reported that AI-CAD-negative cancers had lower BI-RADS scores than positive cancers (p < 0.001), as well as no significant differences in the clinicopathological characteristics between AI-CAD-positive and AI3-CAD-negative cancers.
The study authors suggested that AI-CAD could assist less experienced radiologists in interpreting ABUS images, but cautioned that while AI-CAD findings should be considered for interpreting radiologists, the technology should not be solely relied upon.
The study can be found in its entirety here.