An editorial criticizing the U.S. Preventive Services Task Force (USPSTF) breast cancer screening guidelines has drawn the ire of the American College of Radiology (ACR).
The editorial, published February 5 in the Annals of Internal Medicine, stated that the updated USPSTF guidelines issued in 2023 could create more confusion among women considering undergoing breast cancer screening and make way for more harm tied to screening.
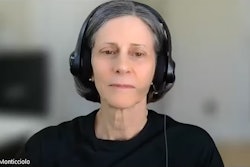
“The USPSTF risks abandoning its role in setting the standard for using evidence and sound judgment to make medical decisions,” wrote Russell Harris, MD, a former USPSTF member, in his editorial. “This would be a loss for all of medicine.”
The USPSTF in 2023 updated its recommendations by endorsing biennial screening with mammography beginning at age 40 for all women. Previously, the task force recommended that women in their 40s make an individual decision about when to start screening. In doing so, the USPSTF upped its recommendation from a C grade to a B grade for women in their 40s.
Harris in his editorial, however, cited randomized controlled trials that influenced the task force’s recommendations in 2002 and 2009 that showed little to no statistically significant reduction in breast cancer mortality in women ages 40 to 49 years. He also wrote that overdiagnosis can be harmful to women. Such harms may include unnecessary biopsy, additional radiation exposure with more imaging, and patient anxiety.
Additionally, Harris wrote that the reason for the 2023 updates in the guidelines came from “a commendable desire” to reduce the disparity of higher breast cancer mortality for Black women. This relied on decision analytic models rather than randomized controlled trials, Harris added.
“Whether mammography effectiveness differs by race, however, has never been tested in a randomized controlled trial,” Harris wrote. “And there was no explanation of how additional screening would reduce the disparity, because current screening rates are higher in Black women than white women.”
He added that the draft recommendation said nothing about individualizing the decision to start screening.
Harris was a member of the RTI International–University of North Carolina Evidence-based Practice Center, where he conducted systematic reviews for the USPSTF from 1997 to 2018. He was also a task force member from 2003 to 2008 and was present at USPSTF meetings which led to updated breast cancer screening recommendations in 2002 and 2009.
The ACR in its February 5 statement said that the editorial “relies on obsolete, hyperbolic information," adding that “most” experts do not support delayed or less frequent breast cancer screening.
The college also said that relying exclusively on randomized controlled trials to inform screening policy “can cost lives.”
“The most recent randomized controlled trial started over 30 years ago. The first [randomized controlled trial] is more than 60 years old. All used outdated, film-screen technology, many obtained only single views of each breast and there were limited screening rounds with variable screening intervals,” the ACR said. “Today, digital mammography with tomosynthesis, which acquires dozens of views of each breast, has increased cancer detection, and a decrease in callbacks and false positives is standard.”
It added that while these trials individually did not have enough statistical power to assess mortality benefit for women getting screened in their 40s, meta-analyses have demonstrated benefit for women in this age group.
The ACR also called the over-screening risks “overstated” and “nonlethal,” and said that high overdiagnosis claims are “not well-founded.”
“So-called false positive exams are usually resolved by the woman coming back to get additional mammographic views, ultrasound or MRI,” the college said. “Anxiety from an inconclusive mammogram result or false positive is brief, with no lasting health effects. Nearly all women who have had a false positive exam still endorse regular screening.”
The full editorial can be found here and the ACR's full statement can be found here.