Lymphoma:
Background:
There are 55,000 to 60,000 new cases of non-Hodgkins
lymphoma (NHL) each year in the U.S. and 24,000 deaths [12]. The incidence of
NHL has been increasing approximately 3%-4% per year for the last three decades
[12]. Hodgkins disease is much less common than NHL with about 7,500 new
cases each year in the United States [12].
Non-Hodgkin's Lymphoma:
Non-Hodgkin's lymphomas represent a heterogeneous group of lymphoreticular malignancies that differ with regard to histopathology, clinical behavioir, response to therapy, and clinical outcome [25]. Treatment for NHL is based on several factors, including tumor grade [12]. NHL is broadly grouped into low-, intermediate-, and high-grade disease subgroups [12]. There is a direct correlation between the degree of FDG uptake and the histologic grade of lymphoma [3]. High-grade tumors demonstrate greater metabolic activity (and greater FDG accumulation) than low grade tumors [4]. In fact, low-grade lesions (including mucosa-associated lymphoid tissue lesions) may not accumulate sufficient FDG to be visualized [16,19].
Low grade NHL accounts for about 40% of new cases. Low-grade lymphomas have an indolent course and most patients are treated with single-agent chemotherapy or conservative watching and waiting [12]. FDG-PET imaging may have only a limited role in managing patients with low-grade lymphoma [12]. As previously mentioned, low-grade lesions (such as MALT lymphomas) are less metabolically active and therefore they may not accumulate significant amounts of FDG resulting in false negative exams [29]. Additionally, the presence of residual disease after treatment may not be clinically relevant as this type of lymphoma generally has no cure, but is indolent with a survival of 10-12 years [12]. PET may play a role in evaluation of these patients should transformation to a higher-grade lymphoma occur (10%-20% of cases) [12].
Intermediate-grade lymphoma accounts for about 40% of new cases and treatment consists of combination chemotherapy and involved-field radiation for patients with bulky disease or early-stage non-bulky disease [12]. The role of FDG-PET imaging in patients with intermediate grade lymphoma would be to demonstrate disease extent and therapy response -- with hopes for improved survival with early modifications in chemotherapeutic regimens.
High-grade NHL accounts for 5%-10% of new cases [12]. Untreated, high-grade NHL is associated with a survival measured in weeks. Treatment consists of aggressive combination chemotherapy [12]. With treatment, remission can be achieved in about 60% of patients [12]. High grade lymphomas are very FDG avid and PET imaging can be used for staging and monitoring response to therapy.
Hodgkin's Disease:
Hodgkin's disease is one of the most common malignant neoplasms in young Americans with 8000 new cases annually [28]. The disease has a bimodal age distribution with a peak in the late 20's and then a second peak after the age of 50 years [28].
For Hodgkins disease, the stage at presentation and tumor cell type determine the patients overall prognosis and optimal method for treatment [28]. Because the anatomic extent of disease is the single most important factor influencing relapse-free duration and overall survival in patients with Hodgkins disease, accurate staging prior to initiation of therapy is essential for proper patient management [2]. The 5 year survival for stages I and IIA are close to 90%, and even in advanced stage disease (stage IVA or IVB) the survival can be as high as 70% [28].
Unfortunately, demonstration of all sites of disease can be
difficult utilizing conventional staging methods. Between 20%-30% of patients
with presumed localized supra-diaphragmatic disease at the time of initial
presentation can be shown to have infra-diaphragmatic disease detected at
staging laparotomy [5]. Unfortunately, laparotomy is invasive and associated
with immediate and potential long-term complications --especially in post-splenectomy
patients. The optimal staging method for lymphoma should be able to
non-invasively identify all sites of disease.
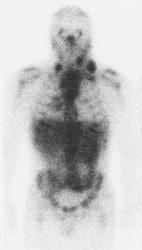
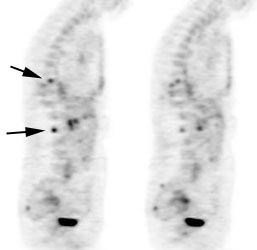
Gallium-67 imaging has been utilized for the evaluation of lymphoma, but the agent suffers from several limitations. First, the gallium exam requires several days to complete (PET exams are performed about 1 hour following injection of the agent). Second, the tumor-to-background ratio is higher for PET than for gallium [29]. Although probably adequate for imaging of the chest, gallium suffers from decreased sensitivity for evaluation of the abdomen due to high physiologic liver and bowl activity [1]. Third, due to its lower anatomic and spatial resolution, gallium imaging has decreased capability to detect small lesions when compared to FDG-PET imaging [1,4]. As a result of these limitations, up to 36% of lesions seen on PET images may not be visible on gallium exams [29]. Also, negative post-therapy gallium scans are not useful unless a pre-therapy scan demonstrating tumor accumulation of the agent were performed [7]. Post-therapy scans can also suffer from non-specific hilar uptake of gallium that can be confused for recurrent disease [8]. Overall, FDG PET exams are more sensitive than gallium imaging in the evaluation of lymphoma patients [22,26].
Gallium scan versus FDG PET exam: The exam on the left is from a gallium scan in a patient with lymphoma. Note the marked amount of background activity and lower spatial resolution compared to a FDG PET exam on an different lymphoma patient (back arrow points to nodal tracer uptake) |
|
PET imaging for lymphoma:
Compared to conventional imaging, FDG-PET imaging has
certain advantages:
1- PET imaging provides a complete body survey which is important when evaluating a multifocal disease process such as lymphoma [2].
2- FDG-PET imaging provides high lesion contrast which permits easy detection.
3- The exam provides very good anatomic localization due to the tomographic nature of the images [2].
4- Lesion detection is based on a biochemical signal (increased metabolism) rather than anatomic criteria [2].
The main trends in healthcare at the present time are increasing cost-effectiveness and decreasing the number of invasive procedures. Non-invasive, metabolic FDG-PET imaging can provide additional information regarding accurate staging, thereby reducing the number of surgical procedures required for staging [8]. PET imaging can also monitor patient response to treatment [8].
PET has been shown to have a major impact on management decisions for lymphoma patients [15]. PET findings can result in a change in patient staging in 8% to 44% of patients (either up-stage or down-stage) [1,4,5,10,15]. FDG-PET exams findings result in a change in patient management in 15 to 62% of patients [15,30]. PET imaging can be positive in up to 50% of patients felt to be in complete remission [15] and the implementation of FDG PET imaging can also result in long term cost savings [4]. Whole-body PET imaging followed by conventional imaging of areas of abnormal FDG uptake has been shown to be more cost effective than a standard conventional staging algorithm [4]. Total management costs were almost half compared with the conventional staging algorithm ($66,292 for conventional staging and $36,250 for FDG-PET staging) [2, 4]. With the advent of PET/CT- coregistered metabolic and anatomic data can be viewed simultaneously [30]. The use of PET/CT has been shown to be more sensitive and specific than CT imaging alone for staging and restaging lymphoma (particularly for organ involvement) [30].
Nodal disease:
PET imaging with FDG has demonstrated high sensitivity for
the detection of abnormal lymph nodes in patients with lymphoma [2]. PET imaging
will generally detect all abnormal lymph nodes identified on CT [1]. Additional
sites of nodal disease are commonly detected, particularly in the abdomen where
CT may miss small mesenteric lymph nodes [1].
Extranodal disease:
Extra-nodal organ involvement (spleen, liver, and bone marrow) carries a worse prognosis when compared to patients with isolated nodal disease [5]. FDG-PET imaging can detect up to 57% more extra-nodal sites of disease than noted on CT scanning [5].
Spleen and Liver Involvement with Lymphoma:
In Hodgkin's disease hepatic and splenic involvement occur
in 3.2% and 23% of patients, respectively [5]. For NHL, hepatic and splenic
involvement are seen in 15% and 22% of patients, respectively [5]. Infiltrative
involvement of the liver, spleen, and bone marrow cannot be accurately detected
on conventional imaging, as organ size is a poor predictor of tumor involvement
[5]. In fact, approximately 30% of patients with splenic enlargement do not have
malignant involvment [5].
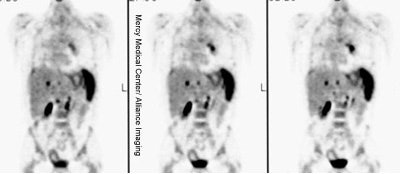
Diffuse splenic involvement: The patient shown below has non-Hodgkins lymphoma. The FDG PET exam demonstrated multiple sites of disease including diffuse involvement of the spleen, focal liver involvement, and persistent sites of adenopathy in the chest and abdomen. Case courtesy of Mercy Medical Center Alliance Imaging, Dr. Steve Allen. |
|
FDG PET imaging is more accurate than CT for the detection of lymphomatous involvement of the spleen [5,27]. On FDG PET imaging, diffuse or focal splenic uptake of greater intensity than the liver is felt to represent tumor involvement [27]. Infiltrative lymphomatous involvement of the spleen can be detected with a 67% increased frequency when compared with CT imaging [5]. Hepatic tumor involvement is characterized by focal or diffuse increased tracer accumulation [5].
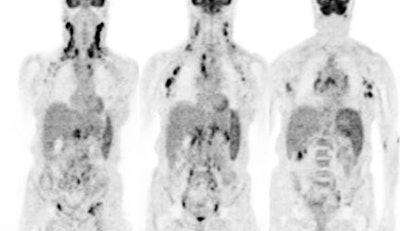
Diffuse lymphoma: In the case below, FDG PET imaging was performed prior to conventional imaging for patient staging. There is widespread tracer uptake within adenopathy in the neck, chest, abdomen, and pelvis. The spleen is enlarged and the intensity of FDG uptake is greater than the liver (SUV was 2.5) which is indicative of infiltrative splenic involvement. There was no evidence of osseous disease. (Click image to view rotating cine file) |
|
Liver involvement: The FDG PET study below demonstrates hepatic involvement in a patient with widespread lymhoma. The CT scan in this case was positive. Splenic involvement is also evident on the CT scan and was also present on separate slices (not shown) from the FDG study. (Click PET image to view rotating cine file) |
|
Bone marrow involvement with lymphoma:
Bone marrow involvement indicates stage IV disease and
carries a less favorable prognosis for patients with NHL [11]. Bone marrow
involvement in newly diagnosed lymphoma occurs in 5%-15% (average 10%) of
patients with Hodgkins disease and in 19%- 83% (average 25%) of patients with
NHL [5 6,10,11].
To be detected on CT imaging, osseous involvement needs to
be focal and associated with bone destruction. Patients with infiltrative marrow
involvement demonstrate no bone destruction and are usually asymptomatic [5].
Both focal and infiltrative osseous lesions can be detected on FDG-PET imaging
[5].
Osseous lymphoma: Focal osseous involvement of the spine was identified in this patient with lymphoma. Conventional images were negative. |
|
Infiltrative osseous involvement appears as generalized increased tracer activity greater than the liver within the bone marrow [5,24]. Lymphomatous involvement of the bone marrow can be detected on FDG-PET with a sensitivity of 81%- 88%, and a specificity of 100% [1, 6, 10]. In comparison to 99mTc-MDP bone scintigraphy, FDG-PET imaging has been shown to be superior for the evaluation of osseous involvement by lymphoma [9]. FDG imaging can detect up to 42% more osseous lesions than 99mTc -MDP bone scintigraphy [9].
Bone marrow biopsy (bilateral posterior iliac crests)
represents the standard diagnostic procedure to confirm bone marrow involvement
[6]. Unfortunately, bone marrow biopsy samples only a small volume and is
associated with a high rate of false-negative findings (due to patchy or
localized marrow involvement) that may lead to errors in patient management [6].
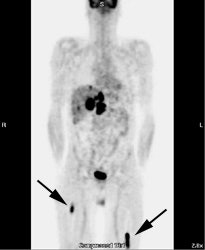
Osseous lymphoma: Unsuspected focal osseous involvement of the femurs was identified on PET imaging of this patient with newly diagnosed B-cell non-Hodgkin's lymphoma (black arrows). Extensive hepatic involvement was seen within the abdomen, but there were no other sites of bone disease. Focal bone disease such as this will not be detected on bone marrow biopsy. |
|
In one study, PET imaging revealed osseous involvement not detected on bone marrow biopsy in 12.8% of patients [6]. This finding resulted in an increase in patient stage in 10% of patients [6]. In that same study, bone marrow biopsy revealed tumor involvement in 5% of patients that was not detected by FDG-PET imaging [6]. However, the cases in which FDG-PET was false negative involved low- or intermediate-grade lymphomas with only discrete displacement (up to 10%) of normal marrow [6]. Because the degree of FDG uptake declines in a lower grade of malignancy -- the combination of lower numbers of malignant cells and low FDG tumor uptake likely resulted in low marrow activity [6].
Other applications for PET imaging in the evaluation of lymphoma include: Assessment for tumor recurrence, differentiate scar from residual tumor mass, and to monitor response to therapy and predict outcome.
1- Assess for tumor recurrence: PET provides a rapid whole body survey to assess for recurrent disease.
Recurrent lymphoma: The patient shown below had a history of submandibular lymphoma and presented for the evaluation of right hip and back pain. CT imaging revealed evidence of recurrent lymphoma, but failed to identify the lesion in the right psoas muscle which was likely the cause of the patient's pain (black arrow on FDG PET exam). Case courtesy of CTI PET Systems, Inc. |
|
2- Monitor response to therapy and predicting outcome:
Following completion of first-line chemotherapy: Obtaining a complete remission is the main objective of first-line chemotherapy because it is usually associated with a longer progression-free survival compared to a partial remission [25]. Conventional imaging modalities such as CT and MR are capable of demonstrating only decrease in lesion size and are poor predictors of clinical outcome following treatment for lymphoma [18]. On long-term follow-up, 50% or fewer of patients with positive CT findings have disease relapse or other evidence of residual tumor [18].
Currently, FDG PET is considered to be more accurate than anatomic imaging modalities in assessing treatment effects [19,25]. On PET imaging, FDG activity reflects the mass of viable cells within a tumor [4]. Following initiation of chemo or radiation therapy, changes in tumor metabolism occur prior to any significant decrease in tumor mass (size) [4]. Persistent FDG uptake after completion of chemotherapy is an indication of lack of tumor response and is associated with a shorter progression-free survival [19,20,21,23,28]. In patients with positive FDG PET scans following completion of first-line chemotherapy, relapse can be observed in 62% to 100% of patients [19,20,25,28]. A negative PET scan following therapy is associated with a much lower risk of relapse (4% to 16%) and a longer disease free survival [19,20,25,28]. In a study of patients with Hodgkin's disease following completion of therapy [28], the overall diagnostic accuracy of FDG PET imaging for the prediction of disease relapse was 92%, compared to 56% for conventional CT imaging [28]. PET had an overall sensitivity of 79%, a specificity of 97%, a positive predictive value of 92%, and a negative predictive value of 92% [28]. In this study, 92% of patients with a positive PET scan following therapy, had a relapse detected on follow up imaging [28]. Three patients with negative post-therapy scans did eventually relapse, but the time to relapse was approximately 1 year [28].
Early prediction of response to therapy: Studies are exploring the early implementation of FDG PET imaging to assess for treatment response. Early assessment of response to chemotherapy can help to avoid the toxicity and cost of ineffective treatment [4]. Second-line therapy can then be instituted early to maximize the patients potential for cure [4, 17]. A significant decrease in FDG uptake can be seen as early as one day following initiation of chemotherapy (therefore baseline scanning must be performed prior to institution of therapy) [31].
FDG-PET imaging performed after completion of the first course of chemotherapy can provide important information regarding treatment outcome [17]. Early data indicates that following effective chemotherapy, there is a rapid decrease in metabolic activity within the tumor (a decrease in SUV between 75%-90% within 7 days of initiation of therapy) [4]. Patients that demonstrate persistent positive FDG exams after one cycle of chemotherapy are at a greatly increased risk for subsequent disease relapse [17]. Recurrent disease occurred in 90% of patients with positive FDG exams after their first course of chemotherapy [17]. Conversely, 85% of patients with negative FDG exams after one course of therapy remained in remission after a minimum follow-up of 18 months [17].
Persistent positive FDG exams after one cycle of chemotherapy likely reflect metabolic activity within potentially resistant clones, which do not respond to treatment as quickly as chemosensitive cells [17]. Imaging after one course of chemotherapy was also more accurate than imaging following completion of therapy for predicting outcome (87% versus 70%) [17].
When monitoring patients for response to therapy it is important to remember that there are statistical variations in tumor SUV measurements. Repeat measurements of the same lesion can vary by 8%-14% [14]. Changes of greater than 25% cannot be explained by statistical variations alone and should be considered to represent a definite change in metabolism [14].
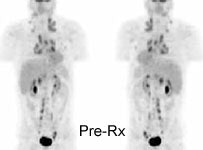
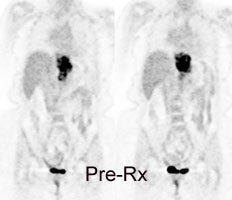
Monitor response to therapy in lymphoma: The patient shown below was a 29 year old male with a history of recurrent lymphoma despite chemotherapy and stem cell transplant. The patients initial PET scan (left) demonstrated extensive nodal disease throughtout the neck, chest, abdomen, and pelvis. The patient was treated with a repeat stem cell transplant. A post-treatment FDG PET exam demonstrated interval resolution of previously identified sites of disease consistent with a response to therapy. Note renal collecting system activity on both studies. The exams were performed on a Siemens ECAT EXACT PET scanner (manufactured by CTI). Case courtesy of North Texas Clinical PET Institute, Dallas, Texas and CTI PET Systems, Inc. Click images to view cine avi file (230K) |
|
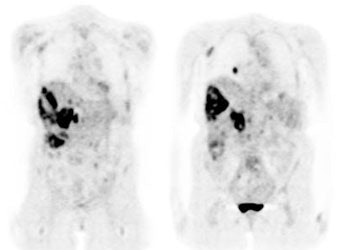
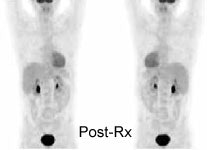
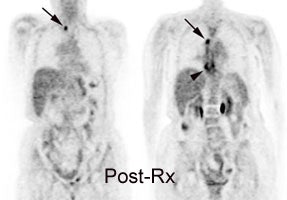
Monitor response to therapy in lymphoma: The patient shown below is a teenage male with Hodgkins disease. The pre-therapy scan confirmed disease only above the diaphragm. The post-therapy scan was performed following two cycles of chemotherapy and demonstrated complete resolution of all sites of disease. Early data indicates that following effective chemotherapy, there is a rapid decrease in metabolic activity within the tumor. Click images to view rotating avi files (note para-cardiac and costophrenic angle nodes can also be seen on these images). |
|
|
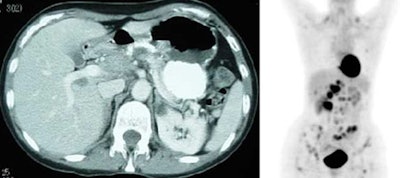
Monitor response to therapy in lymphoma: The patient shown below had a history of Hodgkins lymphoma and had undergone stem cell transplant. A follow-up CT scan revealed increased soft tissue in the region of the porta hepatis which was suspicious for adenopathy, but the patient's lack of internal fat limited the CT evaluation. The patients FDG PET exam revealed widespread intra-abdominal, pelvic, and inguinal adenopathy consistent with extensive recurrent lymphoma which was not appreciated on the CT exam. Case courtesy of CTI PET Systems, Inc. |
|
|
3- Differentiate scar from residual tumor mass: A residual mass after treatment of lymphoma is a clinical challenge because it may represent residual viable tumor or tissue fibrosis [7]. Unfortunately, there are no reliable radiographic characteristics that permit differentiation between malignant and fibrotic tissue. A delay in the diagnosis of residual disease can result in a loss of precious time prior to institution of salvage therapy [23].
FDG will accumulate in viable tumor, but does not accumulate in fibrotic or necrotic tissue [4]. In patients with lymphoma, between 30% to 64% will exhibit a residual mass following completion of therapy [4,23,25]. However, only 18% of these patients will eventually relapse [7,19].
FDG accumulation within a residual mass is associated with a higher predictive value for relapse and an overall worse survival compared to patients without FDG uptake [7,23]. The disease-free survival at one year for PET-negative and PET-positive patients at one year has been reported to be 95% and 40%, respectively [23]. Persistent metabolic activity within a residual mass should prompt strong consideration for additional therapy [7], although in some cases the uptake may be related to thymic hyperplasia or a histiocytic reaction [23]. On long term follow-up, between 16% to 25% of patients with negative PET scans and a residual mass do eventually relapse [7,23], however, the relapse occurs in another site in up to 80% of these cases [7].
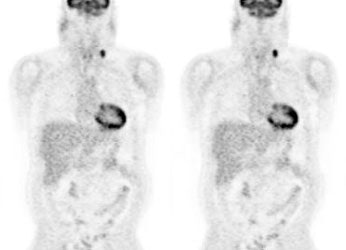
Residual mass post-therapy: The patient shown below had received chemotherapy for lymphoma. There was a residual left neck mass following completion of therapy. A FDG PET exam revealed persistent metabolic activity within the mass concerning for residual tumor. Based upon the FDG exam findings, the patient's management was changed to include additional chemotherapy. |
|
|
Limitations of FDG PET Imaging in Lymphoma:
False-positives exams have been reported in association
with non-specific inflammatory lymph nodes and this can potentially result in
incorrect patient staging [1, 2]. However, it should be pointed out that
conventional imaging could also produce false-positive exams when a reactive
enlarged node is classified as involved with tumor. Lack of increased metabolic activity within enlarged nodes has been shown
to correlate with lack of tumor involvement [4].
Small lesions (under 1 cm in size) may lack sufficient
metabolic activity to be properly identified [2]; however, using this size
criterion, nodes less than 1 cm in size would also not be characterized as
abnormal by conventional imaging.
PET imaging can be degraded by physiologic activity that
can mask lesions -- although to a much lesser degree than gallium scintigraphy.
The brain has intense uptake of FDG and may obscure a central nervous system
(CNS) lesion. As standard staging with CT does not usually include the brain,
the decreased sensitivity of FDG-PET for this region is not a true limitation of
the exam. With either conventional or PET staging, concern for CNS involvement
would require further evaluation with MR imaging.
Cardiac uptake is high in a post-prandial state, and
therefore patients should be fasting to minimize myocardial uptake and maximize
evaluation of the chest. Renal and bladder activity (due to urinary excretion)
may obscure abnormalities in the abdomen. Faint bowel activity can also be seen
on FDG exams, but is generally not enough to cause confusion with actual
disease.
REFERENCES:
(1) Radiology 1997; Moog F, et al. Lymphoma: role of whole-body
2-deoxy-2-[F-18]fluoro-D-glucose (FDG) PET in nodal staging. 203: 795-800
(2) J Nucl Med 1997; Hoh CK, et al. Whole-body FDG-PET imaging for staging of Hodgkin's disease and lymphoma. 38: 343-348
(3) J Nucl Med 1999; Delbeke D. Oncological applications of FDG PET imaging: Brain tumors, colorectal cancer, lymphoma, and melanoma. 40: 591-603
(4) Clinical Positron Imaging 1998; Romer W, et al. Positron emission tomography in diagnosis and therapy monitoring of patients with lymphoma. 1 (2): 101-110
(5) Radiology 1998; Moog F, et al. Extranodal malignant lymphoma: Detection with FDG PET versus CT. 206: 475-481
(6) J Clin Oncology 1998; Moog F, et al. 18-F-Fluorodeoxyglucose-positron emission tomography as a new approach to detect lymphomatous bone marrow. 16 (2): 603-609
(7) Blood 1999; Jerusalem G, et al. Whole-body positron emission tomography using 18-F-Fluorodeoxyglucose for post-treatment evaluation in Hodgkin's disease and non-Hodgkin's lymphoma has higher diagnostic and prognostic value than classical conventional tomography scan imaging. 94 (2): 429-433
(8) Acta Oncol 1999; Bangerter M, et al. Positron emission tomography with 18-Fluorodeoxyglucose in the staging and follow-up of lymphoma in the chest. 38 (6): 799-804
(9) J Nucl Med 1999; Moog F, et al. FDG PET can replace bone scintigraphy in primary staging of malignant lymphoma. 40 (9): 1407-13
(10) Ann Oncol 1998; Bangerter M, et al. Whole-body 2-[18F]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for accurate staging of Hodgkin's disease. 9 (10): 1117-22
(11) Clin Nucl Med 2000; Lee J, et al. Dichotomy between Tc-99m MDP bone scan and Fluorine-18 fluorodeoxyglucose coincidence detection positron emission tomography in patients with non-Hodgkin's lymphoma. 25: 532-535
(12) J Nucl Med 2001; Segall GM. FDG PET Imaging in patients with lymphoma: A clinical perspective. 42: 609-610 (No abstract available)
(13) J Cancer Res Clin Oncol 2000; Ilknur AK, et al. Positron emission tomography with 2-[18F] fluoro-2-deoxy-D-glucose in oncology: Part II: The clinical value in detecting and staging primary tumours. 126: 560-574
(14) Blood 1998; Romer W, et al. Positron emission tomography in non-Hodgkin's lymphoma: Assesment of chemotherapy with fluorodeoxyglucose. 91: 4464-4471
(15) J Nucl Med 2001; Schoder H, et al. Effect of whole-body 18F-FDG PET imaging on clinical staging and management of patients with malignant lymphoma. 42: 1139-1143
(16) Radiol Clin N Am 2001; Delbeke D, Martin WH. Positron emission tomography in oncology. 39: 883-917
(17) J Nucl Med 2002; Kostakoglu L, et al. PET predicts prognosis after 1 cycle of chemotherapy in aggressive lymphoma and Hodgkin's disease. 43: 1018-1027
(18) J Nucl Med 2002; Lowe VJ, Wiseman GA. Assessment of lymphoma therapy using 18F-FDG PET. 43: 1028-1030 (No abstract available)
(19) J Nucl Med 2003; Kostakoglu L, Goldsmith SJ. 18F-FDG PET evaluation of the response to therapy for lymphoma and for breast, lung, and colorectal carcinoma. 44: 224-239
(20) Br J Haematol 2001; Naumann R, et al. Prognostic value of positron emission tomography in the evaluation of post-treatment residual mass in patients with Hodgkin's disease and non-Hodgkin's lymphoma. 115: 793-800
(21) Leukemia 2002; Becherer A, et al. Positron emission tomography with [18F]2-fluoro-D-2-deoxyglucose (FDG-PET) predicts relapse of malignant lymphoma after high-dose therapy with stem cell transplantation.16:260-7
(22) Oncol Rep 2002; Shen YY, et al. Comparison of 18F-fluoro-2-deoxyglucose positron emission tomography and gallium-67 citrate scintigraphy for detecting malignant lymphoma. 9:321-5
(23) Blood 2001; Weihrauch MR, et al. Thoracic positron emission tomography using 18F-fluorodeoxyglucose for the evaluation of residual mediastinal Hodgkin disease. 98:2930-4
(24) GE PET Masters Series Clinical PET; Delbeke D. Verbal communication. Sept 18-20, 2002J
(25)J Clin Oncol 2001; Spaepen K, et al. Prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F] FDG) after first-line chemotherapy in non-Hodgkin's lymphoma: is [18F] FDG-PET a valid alternative to conventional diagnostic methods? 19: 414-419
(26)Radiology 2003; Bar-Shalom R, et al. Camera-based FDG PET and 67Ga SPECT in evaluation of lymphoma: comparative study. 227: 353-360
(27) J Nucl Med 2003; Rini JN, et al. 18F-FDG PET versus CT for evaluating the spleen during intial staging of lymphoma. 44: 1072-1074
(28) J Nucl Med 2003; Guay C, et al. Prognostic value of PET using 18F-FDG in Hodgkin's disease for posttreatment evaluation. 44: 1225-1231
(29) Radiology 2004; Rohren EM, et al. Clinical applications of PET in oncology. 231: 305-332
(30) Radiology 2004; Schaefer NG, et al. Non-hodgkins lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging- do we need contrast-enhanced CT? 232: 823-829
(31) J Nucl Med 2004; Yamane T, et al. Decreased 18F-FDG uptake 1 day after initiation of chemotherapy for malignant lymphoma. 45: 1838-1842