The hybrid OR suite, page 3
Boom design
Another aspect that required a lot of careful thought and discussion was the installation of the booms. A guiding principle of the project set forth by the executive project team was to avoid having cords and cables sprawling across the floor of the suites. Anesthesia machines and ancillary equipment such as patient warmers, etc., are mounted on booms. This decision, coupled with the decision to install an Artis Zeego device (Siemens Healthcare), created a very complex reflective ceiling plan (RCP).5 (An RCP shows a view of the room as if looking down through the ceiling at an imaginary mirror 1 ft below the ceiling level, showing the reflected image of the ceiling above.)
The Zeego device requires a "no-fly zone" -- an area on the ceiling with no fixed equipment that would interfere with its movement. Between the surgical lights to support open procedures, the no-fly zone, all the anesthesia equipment, and the dual imaging monitors being mounted on booms, the planning became very complex. Specific protection stops were installed as necessary on many of the booms to avoid collisions, and several codesign sessions between the respective stakeholder groups were held to harmonize the boom design.
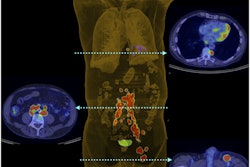
 Figure 4: Final design: Note the use of color-coded floor zones to indicate relative risks of radiation, and guidance for equipment placement.
Figure 4: Final design: Note the use of color-coded floor zones to indicate relative risks of radiation, and guidance for equipment placement.Simulation exercises prior to opening
The hybrid OR team went through several rounds of simulation training to error-proof the workflow before opening the new rooms for procedures. Beginning with a mock-up of operating rooms, including mock-ups of the placement of critical equipment in the hospital's parking garage, we were able to define the movement of patients into the operating room and from the beginning to end of specific procedures. We were then able to model each aspect of the typical endovascular, open, and hybrid case. Through these exercises, we identified setup issues and worked to remove workflow constraints.
The simulations provided a safe way for the interventional and surgical teams to fine-tune the workflow, and they allowed us to identify potential problems that were not evident from the design documents alone. For example, the team revised the circulation patterns for nurses and technologists when circulating for supplies for our physicians. Another example of circulating refinement was optimization of the locations of in-room movable equipment.
Supporting technologies
Managing supplies is an ongoing challenge in procedural areas, with the twin goals of never being out of something (stock out) but not having so much on hand that it gets in the way or leads to costly overstocking and expirations. The radiology team had had several years of experience with a radiofrequency identification device (RFID)-based secure supply chain management system for managing the ordering, usage, and tracking of the majority of the high-priced interventional supplies in 2006.6 By this prior experience, the RFID system was shown to be of significant help in eliminating waste and in more accurately capturing supply usage. We decided to install the RFID-enabled supply management system in the four hybrid suites.
The RFID system receives an automated feed from with the RIS scheduling application. This ensures the correct patient and session are identified with a unique accession number for the case. With a patient selected from the worklist, several automated events occur simultaneously each time a product is removed from one of the cabinets.
These events include the following:
- Association of the product to the patient's record for implant tracking
- Charge capture through a connection with the RIS
- Decrement of the on-hand count
- An auto reorder message to the purchasing system
- The addition of a summary message of all items used to the physician's report
The system also allows for automatic transmission of messages to managers regarding expired products, aging products, and recalls.
While the radiology team was well-versed with the RFID technology, it still required collaboration between stakeholders to define par levels and to train staff unfamiliar with the system.
Conclusion
The planning, design, and implementation of the four new hybrid OR suites at MGH's Lunder Building required two related and intertwined processes, one technical and one cultural:
- The technical challenges involved managing trade-offs that stem from attempting to merge technologies designed for different purposes into a single, flexible system. The goal was to make the best use of both and to allow for rapid transition, when necessary, from one technology to another fairly easily to support two very different services. The selection of a breakable table with accompanying trolley system is one example, and the "quick connect" box is another.
- The cultural challenge involved ensuring that the hybrid team would have the right mix of skills, competencies, and ability to work together in new and unfamiliar ways.
The development process was a useful learning experience for the hospital, leaving us not only with enhanced capacity for state-of-the-art patient care, but also increased confidence in our ability to manage similar challenges that will certainly arise in the future.
Co-authors Robert Sheridan, Maureen Hemingway, Lai Kuen Morrison, Dr. Joshua Hirsch, and Dr. James Thrall are from Massachusetts General Hospital in Boston. Correspondence: Lai Kuen Morrison, email: [email protected], telephone: 617-724-5332.
References
- Frankel AS, Leonard MW, Denham CR. Fair and just culture, team behavior, and leadership engagement: the tools to achieve high reliability. Health Serv Res. 2006;41(4 Pt 2):1690-1709.
- Page SE. The Difference: How the Power of Diversity Creates Better Groups, Firms, Schools, and Societies. Princeton, NJ: Princeton University Press; 2007.
- Hill LA, Travaglini M, Brandeau G, Stecker E. Unlocking the slices of genius in your organization: leading for innovation. In: Nohria N, Khurana R, eds. Handbook of Leadership Theory and Practice. Boston: Harvard Business Press; 2010.
- Moore GE. Cramming more components onto integrated circuits. Proceedings of the IEEE. 1998;86(1):82-85.
- WikiHow. How to read a reflected ceiling plan. http://www.wikihow.com/Read-a-Reflected-Ceiling-Plan. Accessed on June 5, 2014.
- Byers E, Gomez MA, Sheridan RM, Orr NW, Hirsch JA. Radiofrequency identification for inventory in neurointerventional practice. J Am Coll Radiol. 2011;8(3):191-198.
1 | 2 | 3 | Previous page