Minnies finalists, page 2
Best Radiologic Technologist Training Program
This year's competition for the Best Radiologic Technologist Training Program is a battle between two programs that have long histories in this category of Minnies. Johns Hopkins has won the top honor seven times in the 20 years that the Minnies have been held, while Thomas Jefferson University has won twice, most recently in 2017.
Johns Hopkins University, Baltimore, MD
 Johns Hopkins University.
Johns Hopkins University.The Johns Hopkins Schools of Medical Imaging offers programs in radiography, nuclear medicine technology, and diagnostic medical sonography. Sandra Moore is the director of the schools.
The radiography program is an 18-month full-time program that leads to a certification in diagnostic radiography; the nuclear medicine program likewise runs a year and a half and also offers experience in CT. Finally, the diagnostic medical sonography program runs 18 months and offers training in both general and specialized sonography procedures.
In addition to the main programs, Johns Hopkins offers postprimary programs in CT as part of a five-month program that can be attended as a paid hired position or under a tuition option. The university's MRI program is a six-month term.
Thomas Jefferson University, Philadelphia, PA
 Thomas Jefferson University.
Thomas Jefferson University.The Minnies winner in 2017 in the Best Radiologic Technologist Training Program category, Thomas Jefferson University highlights the fact that its program offers both bachelor's and master's degrees in radiological sciences. The university believes that these options give graduates more flexibility when they enter the workforce and better chances for advancement.
The university's full-time Bachelor of Science track consists of one concentration for 12 months or a dual concentration for 24 months. The program integrates components of didactic, laboratory, and clinical education into its curriculum. Classroom work is concentrated into early semesters, while clinical rotations increase over time.
Thomas Jefferson highlights hands-on experience with state-of-the-art equipment, as well as the program's 95% to 100% career placement rate since 1995, and the 85% pass rate on certification exams for all imaging concentrations. The program's attrition rate is less than 10%.
Most Significant News Event in Radiology
Core Exam "fail" rate rises to highest level in seven years

Has the radiology board exam become too difficult? That's question that was raised after the American Board of Radiology (ABR) reported that 15.9% of radiologists who took the exam in June failed the test -- the highest rate since the new Core Exam format was implemented in 2013.
Fallout from the high "fail" rate has reverberated throughout radiology and has raised tensions between the ABR, which wants a test that will be a realistic reflection of knowledge and comprehension of radiology, and radiologists-in-training, who see the exam as a high-stakes hurdle that must be passed at any cost.
Ironically, the ABR adopted the Core Exam seven years ago to improve on the old oral-based board exam, which was seen as being too subjective to the whims of individual reviewers. Now, residents take a computerized test over two days that is supposed to be an improvement by testing their knowledge on a wide range of topics in a more standardized fashion.
But the accusation now is that the new test simply promotes the rote memorization of radiology factoids that have little relationship to the work that an actual radiologist does. The ABR cast shade on the use of test-preparation tools in a recent letter, but the suggestion prompted pushback in the AuntMinnie.com Forums by many observers who charged that the ABR itself had developed a test emphasizing knowledge of esoterica over actual clinical skills.
"If we are able to get the finding, make a meaningful diagnosis, and function as a radiologist, does it *truly* matter if someone may not know the specifics about piezoelectric expansion of crystals in an ultrasound probe or the intricacies of reception bandwidth in reference to a type of artifact?" one poster wrote.
Growth of artificial intelligence and machine learning in radiology
Will artificial intelligence (AI) be the Most Significant News Event in Radiology in the Minnies for the fourth straight year? The fact that AI is still a hot topic after so many years illustrates the hold that the technology has on radiology's psyche.

For the most part, radiology has moved past the "fear" stage of AI, with most radiologists coming to embrace the technology as a welcome helping hand to assist with an ever-burgeoning volume of clinical data. There are signs, however, that medical students have not gotten the message, and some are said to be reticent about entering a field in which robots could be reading scans in years to come.
Ironically, many prominent radiologists are coming to the conclusion that the most exciting use cases for AI won't be in image interpretation at all but rather in helping with issues such as data processing, including enhancing CT image acquisition with less radiation dose and higher image quality.
Having said all that, radiologists are still waiting for AI to make a real clinical impact, with few algorithms in use in a real-world clinical environment. And questions continue to be raised about the validity of research studies claiming that AI algorithms perform on par with actual humans.
Biggest Threat to Radiology
There is good news and bad news behind this year's candidates in Biggest Threat to Radiology category. The good news is that for the first time in five years, "Commoditization of radiology services" will not be named radiology's greatest threat. The bad news is that this year's finalists aren't held in much higher esteem by most radiologists.
Corporate takeovers of independent radiology practices

Radiologists have always prided themselves on their independence. While they provide service for some of the largest health systems in the country, the traditional business model has been for radiologists to form together in private-practice groups, where they remain masters of their own destiny.
That's all started to change. The rise of corporate radiology companies -- which have oftentimes grown by acquiring smaller groups -- is turning many radiologists from entrepreneurs into employees. Meanwhile, hospitals continue to expand by swallowing up outpatient centers that once operated independently.
The trend has even become so profound that some pundits are talking about -- gasp! -- forming a union to help radiologists represent their interests and negotiate with larger entities.
But in many other cases, private practices are deciding it's easier to switch than fight -- and are taking the easy money from corporate firms rather than continuing to swim against the tide.
And with the shift may come a change in attitudes. Will the new breed of radiologist-employee five or 10 years from now continue to see corporate takeovers as a threat -- or will they be perceived as an opportunity? Only time will tell.
Physician burnout

A relatively new arrival in the Minnies, physician burnout is a problem plaguing not just radiology but also healthcare as a whole. One study found that burnout was costing the U.S. healthcare system nearly $5 billion physician turnover and reduced clinical hours.
Within radiology, a recent study found that some 77% of radiology practice leaders believed that burnout was either a significant or very significant problem. At the same time, few practices (19%) reported that they had tools in place to address physician burnout.
What's driving burnout? Some have blamed growing economic pressures on physicians; others have pointed the finger at information technology, which they believe has been pushing physicians from a traditional role as healers to being essentially button pushers and data-entry clerks.
But fortunately, recognition of the burnout problem has also spurred a search for solutions -- the first of which is acknowledging that the problem exists in the first place.
Hottest Clinical Procedure
3D printing of internal anatomical structures
Winner in the Hottest Clinical Procedure category in the 2016 and 2017 editions of the Minnies, 3D printing of internal anatomic structures is back in the running in the 20th year of the awards event.
Perhaps that's because researchers continue to find new uses for 3D printing. By giving users the ability to visualize and interact with structures they can touch and feel, 3D-printed models are invaluable for planning surgical procedures, informing patients about operations, and educating medical students and residents.
For example, researchers from the University of Michigan found that 3D models based on CT scans helped them customize implants required for repairing fractures of the eye socket. Meanwhile, a group from Australia built a 3D model of a human head for simulating neurosurgical procedures.
In fact, 3D models have the potential to be used for more than just planning and education -- possibly even as bioprinted implants that would replace failed human organs and other structures. For example, researchers at Harvard University published a study on their technique that used 3D printing to create cardiac tissue that was perfusable and that beat consistently for seven days.
PET/MRI
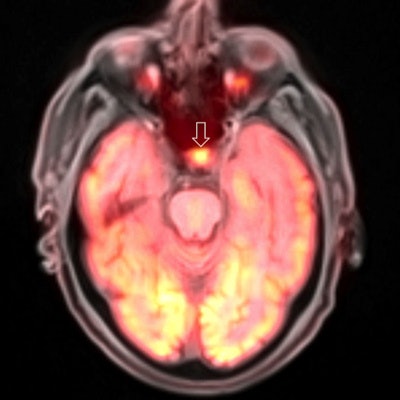 PET/MRI brain scan. Image courtesy of Dr. Ana Franceschi.
PET/MRI brain scan. Image courtesy of Dr. Ana Franceschi.For all its promise, PET/MRI has never been chosen by the Minnies judges as the Hottest Clinical Procedure in radiology.
Perhaps that's because, for all of the "wow" factor entailed by the fusion of metabolic PET images with anatomical MRI scans, the scanners still remain astronomically expensive, far beyond the means of all but the most advanced academic hospital.
One can't help but be impressed by the quality of the images -- but are they clinically useful? One study questioned whether the PET/MRI was really necessary for at least one application: cardiac sarcoidosis. Another found that PET/MRI with a gallium-68 prostate-specific membrane antigen-11 (PSMA-11) radiopharmaceutical was equivalent to other tools for assessing the progression of prostate cancer -- making one wonder why it's worth the extra expense at all.
Perhaps PET/MRI simply needs a killer use case, the one application for which it and it alone is uniquely suited. PET/MRI may or may not be chosen as the Hottest Clinical Procedure this year, but the fact that it made it to the final round of the Minnies indicates that it's occupying a growing share of radiology's attention.
Previous page | 1 | 2 | 3 | Next page