Minnies finalists, page 2
Best Radiologist Training Program
The 2020 competition for Best Radiologist Training Program pits two heavyweights of higher education against each other: Stanford University and Harvard University's Massachusetts General Hospital. These two institutions are used to trading off the No. 1 spot on everything from college rankings to the number of graduates on the Forbes "30 under 30" list. But which program is best for radiologist training?
Massachusetts General Hospital, Boston, MA
 Massachusetts General Hospital. Image courtesy of MGH.
Massachusetts General Hospital. Image courtesy of MGH.In 1915, Massachusetts General Hospital (MGH) became the first hospital in the U.S. to establish a radiology residency program. The imaging department's founder, Dr. Walter James Dodd, was taking chest radiographs at MGH within a year of Wilhelm Conrad Röntgen discovering x-rays.
That commitment to radiology ingenuity continues today. MGH aspires to train the next generation of academic radiologists, and more than 90% of residents pursue subspecialty training.
The radiology department offers both diagnostic and interventional residency programs. MGH boasts a number of cutting-edge imaging technologies available to residents, including an updated PACS, 11 multidetector-row CT scanners, and an inpatient facility with three floors of operating rooms designed for image-guided procedures.
The MGH radiology department also founded an in-house innovation incubator called Medically Engineered Solutions in Healthcare, or MESH. In this first-of-its-kind program, residents can turn clinical ideas into intellectual property that can be licensed and patented.
The program director of the radiology residency program is Dr. Theresa McLoud -- a Minnies semifinalist for Most Effective Radiology Educator in 2020, 2006, and 2005.
MGH has made the semifinals for Best Radiologist Training Program every year since 2002, but the program has only netted a finalist spot one other time, in 2014, when it lost to the American College of Radiology's Radiology Leadership Institute in Reston, VA. Could this be the year MGH finally claims the No. 1 spot?
Stanford University, Stanford, CA
 Stanford University. Image courtesy of Stanford.
Stanford University. Image courtesy of Stanford.Like the surrounding Silicon Valley, Stanford University's Department of Radiology prides itself on innovation. The department touts a commitment to scientific imaging disciplines, including molecular imaging, imaging informatics, nanotechnology, and systems biology.
The department boasts four residency programs, 10 clinical fellowship programs, and six research programs funded by the U.S. National Institutes of Health. Residents can train in diagnostic radiology, interventional radiology, interventional-diagnostic radiology, and a dual program in nuclear medicine and diagnostic radiology.
Recently, the department began shifting resident training from an apprenticeship model to one similar to how airline pilots are trained. This includes using controlled, preselected cases for what the department calls purposeful practice.
In its reimagining of resident training, Stanford introduced a block-conference curriculum, in which residents from different clinical sites meet weekly for a five-hour block conference. The block conference has become quite popular with residents, and the department said it's revising its curriculum to maximize this type of learning.
Stanford is no stranger to contending for the Best Radiologist Training Program title, having appeared in the finals four times and in the semifinals every year since 2003. In a testament to the department's strength, Stanford researchers and educators frequently appear on the list of Minnies laureates.
Stanford's radiology residency program is led by program director Dr. Payam Massaband, a graduate of the program himself. A 2020 win could be especially meaningful to the department, which lost its beloved chair Dr. Sanjiv Sam Gambhir, PhD, to cancer earlier in July. A victory would be the department's first Minnies win in the category since 2009.
Best Radiologic Sciences Program
Duke University and Emory University are the two finalists for Best Radiologic Sciences Program -- with Duke a fresh contender and Emory having previously won the award in 2018.
Duke University, Durham, NC

Duke University offers a unique program called Duke Advanced Radiology Technologist (DART) education, which consists of one- to five-day courses and is directed by Dr. Lynne Koweek and Dr. Daniele Marin. Most of the technologists in the program are from Duke, but DART also accepts technologists from other institutions and even applications specialists from imaging vendors.
Duke launched the program about four years ago to bridge what it saw as a gap in understanding between technologists and radiologists about their respective job roles. For example, DART teaches technologists what radiologists are looking for in an imaging study when it comes to parameters like noise, offers insights into the workflow of a typical radiologist, and the like.
DART offers certified technologists and nurses the opportunity to expand their advanced imaging skills through small group learning as well as hands-on and observational workshops on topics such as MRI body applications, cardiac CT angiography, and dual-energy CT. Duke in particular plays up the fact that DART education is based on actual clinical cases at the institution, which are indicative of the cases that technologists are most likely to see in the real world.
Duke partners with other institutions to provide direct clinical training for nuclear medicine technology, diagnostic medical sonography, and radiologic sciences associate's degrees. It also supports students in securing primary and/or post primary certification from the American Board of Magnetic Resonance Safety, the American Registry of Radiologic Technologists, the Nuclear Medicine Technology Certification Board, and the American Registry for Diagnostic Medical Sonography.
Emory University, Atlanta, GA
Through its four-year Bachelor of Medical Science program, Emory seeks to train radiologic technologists who are both skilled at personal interaction with patients and motivated to engage in a career in diagnostic imaging.
Students synthesize knowledge about anatomy, physiology, and pathology with patient positioning, radiation protection, and image production techniques. The program's curriculum is a mix of classroom and clinical education.
Program participants with or without a current radiologic technologist credential can earn the degree, and they can take advantage of advanced courses like radiology administration, radiography education, and advanced clinical practice in CT and MRI. The course curriculum challenges students to learn effective oral and written communication skills, appropriate patient positioning and radiation safety principles, and how to evaluate images and modify procedures to accommodate patients' needs.
Emory prides itself on a five-year average pass rate on the American Registry of Radiologic Technologists exam of 88.9% (first attempt within six months after graduation) and an average job placement rate of 100% (within 12 months of graduation).
Most Significant News Event in Radiology
As with the rest of the world in 2020, the COVID-19 pandemic had a transformative impact on radiology -- so much so that both finalists for Most Significant News Event in Radiology are different aspects of the novel coronavirus outbreak.
American Board of Radiology postpones 2020 exams
The Core Exam is the first of the certification exams known colloquially as the radiology boards that residents must pass in order to be certified to practice in diagnostic and interventional radiology.
The Core Exam was originally scheduled to take place from May 28 and 29 and June 1 and 2 at testing centers in Chicago and Tucson, AZ. But the arrival of the COVID-19 pandemic prompted the American Board of Radiology (ABR) to announce in March that it was postponing the exams; as the scope of the pandemic widened in June, the ABR said it would be pushing the exams to 2021.
The announcements have had a devastating impact on radiology residents, who follow a carefully choreographed path through their training to studying and taking the boards. Many face the prospect of a one-year delay in entering the radiology workforce.
Indeed, many radiology educators and trainees had hoped that the ABR would be able to find a way to hold the exams remotely in 2020. A coalition of a dozen groups even went so far as to publish an open letter to ABR, urging the group to find alternatives to postponing the exams and noting the personal and professional disruption that a postponement would cause.
Such entreaties were in vain, however, and the ABR in late June said it was sticking to its plan to hold the exams in 2021.
COVID-19 pandemic and its impact on radiology

It's hard to count all the ways in which the COVID-19 pandemic has affected radiology, with the postponement of the board exams being just one facet.
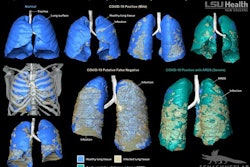
The start of the pandemic saw radiology pressed into service by front-line healthcare workers in Wuhan, China, as a clinical tool to diagnose patients who were coming down with a mysterious respiratory illness caused by a virus that was first called 2019-nCoV, and then renamed SARS-CoV-2. Providers found that CT in particular could be used in cases where reverse transcription polymerase chain reaction (RT-PCR) tests were equivocal.
But controversy soon erupted over how and when to use imaging for the disease that came to be known as COVID-19. Radiology departments recoiled when they realized that using CT to examine patients with COVID-19 also entailed disinfection procedures that could take scanning rooms down for hours at a time.
Fortunately, medical imaging has other tools in its arsenal, including modalities like mobile x-ray and point-of-care ultrasound that can be taken directly to a patient's bedside. While not as sensitive as CT, these tools offer the versatility and portability that CT lacks, so they were pressed into service to triage patients. The question of whether imaging can be used as a first-line tool for COVID-19 diagnosis is one that continues to engender debate.
As the pandemic began to spread beyond the borders of China in late February and March, its ramifications began to ripple in ways that previously had been unthinkable. March is typically the start of the spring conference season, with the European Congress of Radiology (ECR) in early March typically one of the first meetings of the season.
But organizers of ECR 2020 made the courageous decision to call off the meeting just a week before it was to begin, to avoid the uncomfortable prospect of a healthcare conference turning into what we would call now a superspreader event. Other conferences soon followed suit, either postponing their meetings or holding them virtually -- including the Super Bowl of radiology, RSNA.
Radiology soon joined the rest of the world by going into lockdown mode. Ironically, many radiology departments braced for a surge that never came, as patients canceled nonessential exams. This led to drops in imaging volume that varied by 50% to 80%, depending on modality.
The nature of radiology work changed dramatically as well. Fortunately, the discipline had a head start on working at home thanks to teleradiology, which up to now had mostly been used to provide off-hours and subspecialty image interpretations. Teleradiology was soon pressed into service to allow staff radiologists to remain productive while working at home during daytime hours.
Over six months into the COVID-19 pandemic, radiology is still adapting. While some aspects of medical imaging are returning to some semblance of a "new normal," there are indications that disruptions caused by the outbreak are having a major psychological impact on radiologists, causing ills such as insomnia, anxiety, and depression, according to a French survey.
It's anyone's guess how long COVID-19 will continue to cast a shadow over radiology. But odds are that it will also loom large going into 2021 and beyond.
Biggest Threat to Radiology
Burnout of physicians

Physician burnout has become a pervasive issue across healthcare, and radiology is no exception. For the first time, the phenomenon was named Biggest Threat to Radiology in the 2019 edition of the Minnies.
And the problem continued to smolder in 2020 -- in spite of (or perhaps because of) the COVID-19 pandemic. In fact, physician burnout has become so severe that 50% of doctors surveyed in a poll released in January said they would take a pay cut of up to $50,000 annually to reduce their stress -- and that was before the outbreak began.
How bad is the problem in radiology? A study released in August 2019 found that 77% of radiology practice leaders believe that burnout was either a "significant" or "very significant" issue for them. Another study found that while radiologists reported lower levels of burnout than other types of physicians, they also had lower levels of professional fulfillment -- and a higher rate of intention to leave medicine entirely.
And there are signs that the COVID-19 pandemic has made the problem worse. A survey by French researchers released in September found that the outbreak has contributed to insomnia, anxiety, and depression among radiologists.
Could technology come to the rescue? Some radiology key opinion leaders like Dr. Eliot Siegel believe that artificial intelligence (AI) could help by taking the burden of performing redundant tasks off radiologists' shoulders. This concept was reinforced by a study released in December 2019 that found that AI can increase the amount of time that clinicians are able to spend with patients.
Fortunately, some groups are moving to address burnout. A group called the Physician Wellness Academic Consortium (PWAC) was started by Stanford University and has a number of participating academic institutions, with the goal of offering resources to healthcare providers for dealing with the problem.
COVID-19 pandemic and its impact on radiology volumes
The COVID-19 pandemic slammed radiology in 2020, with effects ranging from wiping out the conference schedule for the remainder of the year to forcing the cancellation of radiologist board certification exams.
But it was in radiology exam volume that the outbreak had its biggest effect. As the wave of infections began rising in the U.S. in early March, radiology departments prepared by canceling all imaging exams deemed nonessential -- leading to dramatic drops in exam volume.
The impact was felt across the board, but it varied greatly by modality. Most departments and imaging centers reported at least a 50% drop in overall volume, with mammography and nuclear medicine hit particularly hard. Even hospital inpatient volume fell 17%, according to one survey.
The decline in volume is having a ripple effect across medical imaging. Most radiology vendors reported sharp drops in revenues starting in the second calendar quarter as customers postponed sales, although things appear to have started to rebound in the third quarter. In the end, overall sales of imaging equipment globally should finish down almost 5% compared with 2019, according to one analysis.
How long before the new normal gives way to the old normal, and radiology volume returns to historical levels? That's impossible to say. Many people are still reticent to visit hospitals for fear of infection, and that's prompting public service campaigns urging the public to return for screenings and other nonurgent exams.
But as with the rest of society, radiology may just have to wait until a vaccine for the novel coronavirus becomes available before normalcy can return. And when that will happen is anyone's guess.
Hottest Clinical Procedure
7-tesla MRI
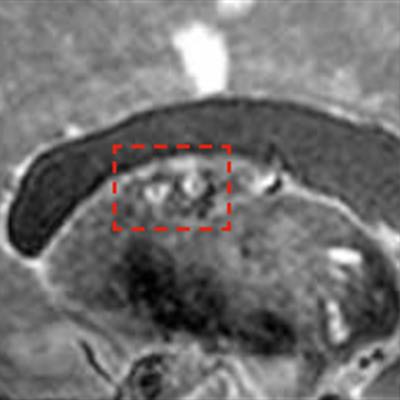 7-tesla MRI can detect the total burden of larger and smaller infarcts. Image courtesy of Dr. Jeroen Hendrikse.
7-tesla MRI can detect the total burden of larger and smaller infarcts. Image courtesy of Dr. Jeroen Hendrikse.Radiology has always been known as the specialty of big iron, and nowhere is the iron bigger than at 7-tesla MRI.
But 7-tesla MRI has always been viewed as a research modality, with the scanners too large, complex, and overpowered to be of use in a clinical setting. Therefore, it's notable that the Minnies expert panel saw enough clinical potential in 7-tesla MRI to vote it into the final round of the 2020 Minnies.
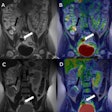
Indeed, researchers and clinicians have been wondering for the past several years whether 7-tesla is ready for the jump to clinical imaging. Assuming you can get one of the beasts sited at your institution, the modality offers improved contrast-to-noise ratio, which translates into exquisitely fine soft-tissue detail.
This can be particularly useful for neurological applications, such as identifying brain structures and pathologies like microinfarcts. For example, researchers at the 2019 European Congress of Radiology found 7-tesla MRI useful for visualizing small pituitary adenomas in patients with Cushing's syndrome -- adenomas that weren't seen on MRI scans at lower field strengths.
Researchers are also looking into the modality's suitability for cardiac imaging. As with the brain, 7-tesla MRI can identify structures not found at lower field strengths, and it could help determine which patients are close to going into heart failure.
But it's not all sunshine and rainbows with 7-tesla scanning. The modality is so powerful that it could require its own set of safety guidelines, according to a group that is working on just that. Unanswered questions include how metallic implants will react at 7-tesla, as well as how to deal with patient reports of vision problems, dizziness, nausea, and vertigo after undergoing scans.
Still, the technology is slowly moving ahead. The first commercial 7-tesla MRI scanner, Magnetom Terra from Siemens Healthineers, was cleared by the U.S. Food and Drug Administration in 2017 (that system incidentally won the Minnie award for Best New Radiology Device in 2015). And in August 2020, GE Healthcare introduced a 7-tesla system of its own, Signa 7.0T, at the 2020 edition of the International Society for Magnetic Resonance in Medicine meeting. Signa 7.0T is pending FDA clearance.
Perhaps the future isn't so far off after all.
3D printing of internal anatomic structures
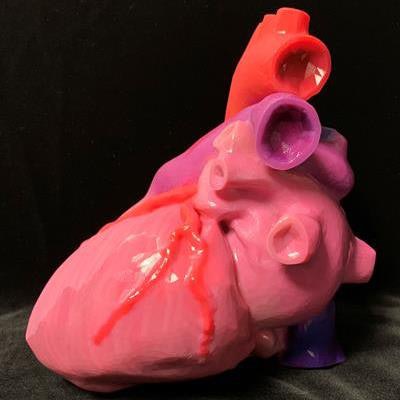 An individually tailored, multicolor 3D-printed heart. Image courtesy of Summer Decker, PhD.
An individually tailored, multicolor 3D-printed heart. Image courtesy of Summer Decker, PhD.At the other end of the spectrum is 3D printing of internal anatomic structures, which has been named the winner in this category in three of the past four years.
Indeed, 3D printing became an essential service in 2020 in response to the COVID-19 pandemic. As a shortage of personal protective equipment became more severe, 3D printing experts found that they could manufacture their own medical supplies, such as face shields.
In the clinical realm, the state of the art in 3D printing advanced significantly in 2020. Researchers found the technology useful for creating 3D-printed surgical guides designed with CT data for total knee arthroplasty procedures, while another group investigated the technology for creating 3D coronary models to develop CT scanning protocols.
But for 3D printing to achieve its true potential, more radiologists will need to be trained on the technology, according to a presentation from RSNA 2019. A program to do just that was established at the University of South Florida, and it's helped radiologists understand the scenarios in which 3D printing is most useful. 3D printing has even been incorporated into the educational curriculum for medical students at the university.
Will 3D printing make it four out of the past five as the hottest technology? Only the Minnies expert panelists know for sure.
Previous page | 1 | 2 | 3 | Next page