3D-printed phantoms of aortic root anatomy offer a noninvasive way to assess the risk of a patient experiencing a leak after transcatheter aortic valve replacement (TAVR), according to a study published in the July issue of JACC: Cardiovascular Imaging.
The study is the first to use 3D printing of models that mimic human tissue to predict TAVR outcomes, wrote a team led by Zhen Qian, PhD, from the Piedmont Heart Institute in Atlanta. The findings could help physicians not only select the best valve type and size for TAVR procedures, but also improve the procedure in patients at risk for valve leaks (JACC Cardiovasc Imaging, July 2017, Vol. 10:7, pp. 719-731).
"Compared with the traditional uses of 3D printing in medicine, such as reproducing patient-specific anatomies, the use of 3D printing as a quantitative tool to study pathophysiology is relatively new," Qian and colleagues wrote. "The relatively fast and inexpensive 3D printing method proposed in this study may provide a better and more practical alternative to computer-based simulations."
Noninvasive technique
One of TAVR's complications after the procedure is paravalvular leak (PVL), in which an inappropriate seal results in blood leaking through the implanted valve and cardiac tissue. Complications occur in 26% to 67% of patients, higher than complication rates after aortic valve replacement, the authors wrote. In turn, PVL is also a risk factor for increased short- and long-term mortality, and although researchers have proposed a variety of methods to predict PVL risk, there is currently no consensus on how best to do so, according to the authors.
 Zhen Qian, PhD, from Piedmont Heart Institute.
Zhen Qian, PhD, from Piedmont Heart Institute.The current study included 18 patients (mean age, 79.6 years) who underwent TAVR between April 2014 and September 2015. Before the procedure, all patients had a contrast-enhanced CT scan; the size of the valve replacement was determined by annular diameter measurements taken by CT. Surgeons implanted the new valves under guidance of fluoroscopy and transesophageal echocardiography (TEE) and evaluated PVL risk (none, trace, mild, moderate, or severe) with TEE after the valve had been placed.
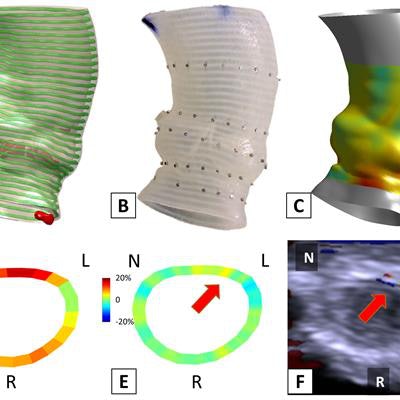
To explore the feasibility of using a 3D-printed phantom to predict the potential occurrence, severity, and location of post-TAVR paravalvular leak, Qian and colleagues developed a printing technique to make models of each patient's aortic root using images acquired at peak aortic valve opening. They then used these models -- along with CT-based strain quantification techniques -- to assess patients' risk of post-TAVR paravalvular leak.
Their main hypothesis was that the uneven distribution of strain in the annulus during TAVR contributes to the occurrence of paravalvular leak; their hope was that the 3D phantoms would help identify annulus strain.
3D modeling of the aortic root took about five to 10 minutes; printing of a batch of 10 phantoms took about 10 hours. Postprint processing took an additional 45 minutes for each phantom, and the cost of printing materials for each was about $200, Qian and colleagues wrote.
They found that annular calcification was a helpful predictor of moderate to severe paravalvular leak immediately after valve placement and before valve dilation by balloon after the procedure, with a sensitivity of 71% and specificity of 82%. But annular strain unevenness, which the group called annular bulge index, was the most accurate in predicting moderate to severe paravalvular leak post-TAVR balloon dilation -- which was conducted in patients with more than a mild risk of the complication -- with a sensitivity of 100% and specificity of 79%.
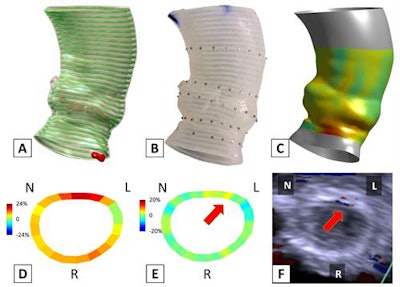 Pre-TAVR CT scans were used to produce the 3D model of the aortic root (A) and the 3D-printed phantom (B). The TAVR prosthesis was deployed in the phantom to simulate the TAVR procedure, from which post-TAVR aortic root strain was quantified in vitro (C, D). The annular bulge index was measured to assess the post-TAVR annular strain unevenness (E), which showed to be predictive of the occurrence, severity, and location of paravalvular leak (F). Image courtesy of Zhen Qian, PhD.
Pre-TAVR CT scans were used to produce the 3D model of the aortic root (A) and the 3D-printed phantom (B). The TAVR prosthesis was deployed in the phantom to simulate the TAVR procedure, from which post-TAVR aortic root strain was quantified in vitro (C, D). The annular bulge index was measured to assess the post-TAVR annular strain unevenness (E), which showed to be predictive of the occurrence, severity, and location of paravalvular leak (F). Image courtesy of Zhen Qian, PhD.Risk assessment
What's the takeaway? 3D-printed phantoms offer a practical way to assess distribution of post-TAVR annular strain -- and therefore estimate paravalvular leak risk, according to Qian's group.
"The annular bulge index is a novel indicator of the post-TAVR annular strain unevenness ... [and it] can be quantified by in vitro TAVR simulation on a patient-specific 3D-printed phantom," the researchers concluded. It "may be feasible to perform procedural simulations on a 3D-printed phantom for pre-TAVR planning, especially in those who are at high risk for post-TAVR paravalvular leak."




















