An automated prostate biopsy system based on real-time guidance with high-field MRI earned high scores for accuracy and image quality, according to a team from J.W. Goethe University in Frankfurt, Germany.
The group concluded, additionally, that using a transgluteal needle approach to the prostate with the patient prone was accurate and safe when used in combination with the pneumatically driven needle positioning system. The transgluteal approach facilitates biopsy in the peripheral zone of the prostate, while avoiding the risk of microbial contamination from the bowel.
Transrectal ultrasonography is the standard initial detection method of prostate tumors in men with elevated prostate-specific antigen (PSA) levels (> 4 ng/mL), and is used for biopsy-guidance imaging exams for patients with elevated PSA levels. However, many patients with elevated PSA levels and negative sextant biopsy do turn out to have cancer at repeat biopsy, driving interest in alternative imaging modalities such as MRI and CT.
In 2005 Dr. Stephan Zangos and his colleagues from Frankfurt published their first results using MR-guided transgluteal biopsy with an open low-field (0.2-tesla) MRI system (European Radiology, April 2005, Vol. 15:4, pp. 174-182).
They examined 25 patients with uncertain or suspicious focal prostate lesions detected by high-field MR of the prostate using an endorectal coil. The procedures were guided using T1-weighted FLASH sequences, using the transgluteal approach. The group used a coaxial technique to biopsy the gland repeatedly (mean 3.8 biopsies per patient) using a 15-gauge pencil tip, with a 16-gauge biopsy handy.
There were no complications or side effects during any of the interventional procedures, which took a mean 11.3 minutes. Pathology revealed 10 cases of hyperplasia or atrophy, three cases of prostatitis, 10 prostate carcinomas, and two cases of normal tissue, the group reported. Two cases of cancer were missed.
In a presentation at the 2007 Computer Assisted Radiology and Surgery (CARS) meeting in Berlin, Zangos discussed his efforts to improve on the group's original results with the aid of a high-field (1.5-tesla) MRI scanner.
"Comparing low-field to high-field MRI -- it's pretty sure who would win," Zangos said. High-field MR-guided biopsy yields high tissue contrast, reliable visualization of prostate lesions as well as the needle, and is easy to perform.
Still, the transgluteal access technique to prostate biopsy is rare. First reported in 1996 by Papanicolau and colleagues from Massachusetts General Hospital in Boston, the researchers used CT guidance to perform transgluteal biopsies of 10 men who had previously undergone colectomy due to ulcerative colitis or colorectal cancer, and as a result had no rectum. Transgluteal biopsy was a "well-tolerated, safe, and effective method" for prostate biopsy in these patients, they concluded (American Journal of Roentgenology, June 1996, Vol. 166:6, pp. 1332-1334).
The MR-compatible assistance system (Innomotion, Innomedic, Herxheim, Germany) includes a scan table, C-arch, guiding arm, and application module (AMO). Planning and control for the interventions are performed outside the scanner room on a desktop PC, which receives DICOM images from the scanner, Zangos said. Servopneumatic drives move the application module to the insertion point. However, the physician has to manually introduce the punction needle.
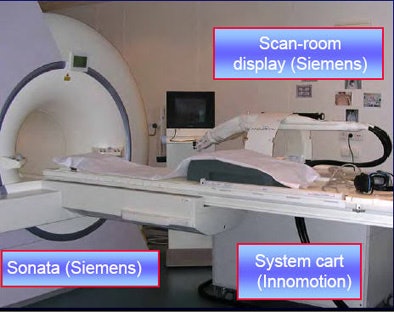 |
| The MR imaging and planning system consists of a 1.5-tesla MRI scanner and viewing equipment (Siemens) and intervention planning system (Innomedic). All images courtesy of Dr. Stephan Zangos. |
 |
Its movements calculated by the external computer, "the guided arm is moved by compressed air," Zangos said. MR images are acquired first for planning and again for the needle insertion.
At the University of Frankfurt Medical Center, the group performed 18 biopsies of patients with prostate lesions using a 1.5-tesla MRI. "We performed biopsies on all patients with abnormally elevated PSA levels, and a negative TRUS-guided biopsy result, presenting a diagnostic dilemma," he said.
 |
| A PC and dedicated software are used to plan the intervention with the MR guidance system. |
The researchers used a spine and loop coil for intervention, while preinterventional imaging was performed with an endorectal coil, Zangos told AuntMinnie.com. "For imaging we prefer T2-weighted TSE sequences and TRUFI sequences," he said. "T1-weighted images were not useful for guidance of the intervention."
T2-weighted sequences are especially useful for prostate imaging because its high tissue contrast properties can help distinguish noncancerous tissues found in prostatitis, dysplasia, and prostatic hyperplasia, from prostate cancer.
The protocol used to monitor the prostate biopsy included T1-weighted fast low-angle shot (FLASH) 2D GRE sequence (TR/TE = 110/4 msec) and T2-weighted turbo spin-echo (TSE) sequences (TR/TE = 3200/97 msec) in transversal orientation.After the position is determined by the planning system, the physician has to manually introduce the biopsy needle, according to Zangos. "We use a normal punction set (designed) for CT biopsies," he said. "You have to be careful when you use something like that because the cannula and surgical knife are ferromagnetic. As you know with MRI, this is the really dangerous part, and you have to keep in mind safety at all times."
The ferromagnetic cannula was used only for adminstering the local anesthesia, while the puncture cannula and biopsy instrument were non-ferromagnetic, enabling easy MR-guidance, Zangos explained.
The patient management protocol included initial MR imaging, laboratory studies of the biopsied tissue, physical examination, infection surveillance, MR-guided biopsy, and observation of the patient for one to two hours following the procedure.
"We have performed MR-guided biopsies in high-field system in 18 patients using the Innomotion assistance systems so far," Zangos said. "Biopsies were performed successfully in 13/14 patients. In one patient we had to stop the use of the Innomotion system due to a technical problem." A modification of the guidance system's software fixed the problem, he said.
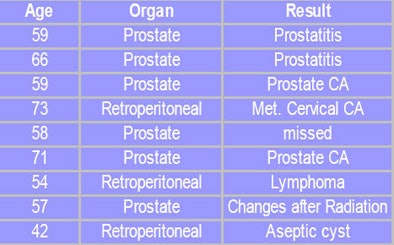 |
| The MRI-based diagnosis corresponded to pathology results in all but one case. |
MRI-guided percutaneous biopsies are feasible, yielding high tissue contrast and high sensitivity for prostate lesions, Zangos concluded. The guidance technique is highly accurate as well, he said. In a gel phantom study published earlier this year, the mean deviation of the needle tip to the target in the phantom was accurate to within 0.35 mm, and the "combination of diagnostic and interventional brings improved results for the patient," Zangos said.
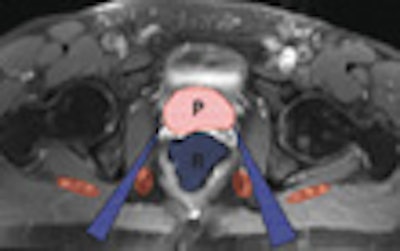
 |
| Future diagnostic systems could incorporate CAD, MRI, MR spectroscopy, and MR-guided prostate biopsy. |
In response to a question from the audience, Zangos said there is, as yet, no mechanism to account for patient movement between the intervention planning and the needle punction, a drawback of the current system.
But movement has not been a problem in the interventions performed to date, all of which were successful, Zangos said. One patient's position had to be adjusted 2-3 mm between the planning and interventional imaging sequences.
By Eric Barnes
AuntMinnie.com staff writer
July 31, 2007
Related Reading
Black men underestimate prostate cancer risk, June 15, 2007
Soy isoflavones may boost efficacy of radiotherapy for prostate cancer June 15, 2007
CARS news: Automated device tracking beats conventional CT/US guidance, June 27, 2007
Electromagnetic navigation aids bronchoscopy biopsy of peripheral lesions, June 13, 2007
Copyright © 2007 AuntMinnie.com