Virtual reality (VR) may be a safer, more time-efficient alternative to conventional fluoroscopy for guiding catheterization, with the potential to increase access to the procedure in rural regions, according to a March 26 presentation at the Society of Interventional Radiology (SIR) 2019 meeting in Austin, TX.
Researchers led by Dr. Wayne Monsky, PhD, from the University of Washington Medical Center used 3D printing and VR technologies to simulate catheter placement in several abdominal and pelvic vessels. They found that VR allowed interventional radiologists to complete catheterization successfully at a much faster pace than with the use of fluoroscopy, both during simulations and for real clinical cases.
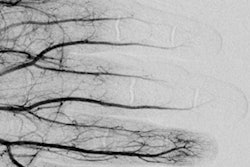
 Setup for simulating interventional radiology procedure on a 3D-printed aorta. All images and video courtesy of Dr. Wayne Monsky, PhD.
Setup for simulating interventional radiology procedure on a 3D-printed aorta. All images and video courtesy of Dr. Wayne Monsky, PhD."Virtual reality will change how we look at a patient's anatomy during an [interventional radiology] treatment," Monsky said in a prepared statement. "This technology will allow physicians to travel inside a patient's body instead of relying solely on 2D, black and white images."
VR reshapes catheterization
An increasing number of groups are showing that VR may be able to facilitate and even improve the efficiency of a wide range of clinical tasks, from detecting obscure lung cancer and guiding glioma resection to correcting MRI segmentation errors.
"We've recently seen virtual reality do incredible things in healthcare, including improving patient experience in the hospital setting, physician training simulations, and presurgical planning," Monsky said. Some of the devices have already received clearance from the U.S. Food and Drug Administration (FDA).
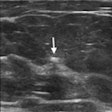
The current standard of practice for catheterization in interventional radiology is to use fluoroscopy, or 2D x-ray image guidance, but this method is limited in the level of detail it can provide, he added. New technologies such as virtual reality could offer improved visualization in 3D without exposing patients and clinicians to radiation, "giving physicians the experience of traveling inside a patient's body and viewing the anatomy in ways never before possible."
Exploring the viability of using VR for catheterization, Monsky and colleagues generated a 3D virtual model of a patient's vasculature based on previously acquired CT angiography scans of the abdomen and pelvis. They used the 3D virtual model to create a 3D-printed model of the vasculature, which they connected to an electromagnetic transmitter that could track the movement of objects in real-time.
This setup allowed clinicians to simulate catheterization using virtual reality instead of typical x-ray guidance. During simulation, interventional radiologists wearing a VR headset were able to insert a catheter with sensors into the 3D-printed vasculature model and watch the catheter as they moved it toward its target.
Virtual reality guides catheter placement for an interventional radiology procedure.
VR offers wider access
To test the efficiency of this technique, the researchers determined the average amount of time it took for an interventional radiologist to simulate catheter placement through the femoral artery and onto three different locations with high precision using VR for guidance.
After 18 simulated procedures, they found that interventional radiologists were able to situate the catheter more than three times faster using the VR technique than when relying on conventional fluoroscopy, for all three targeted vessels. What's more, the interventional radiologists performed the VR simulations an average of five to 10 times faster than they were able to complete catheter placement for similar real-life clinical cases.
| Time required for catheterization using different IR techniques | |||
| Targeted vessel | Real clinical case | Fluoroscopy simulation | VR simulation |
| Right hepatic artery | 188.4 sec | 73.5 sec | 22.6 sec |
| Gastroduodenal artery | 171.2 sec | 70.3 sec | 17.6 sec |
| Splenic artery | 92.3 sec | 66.1 sec | 18.6 sec |
The improved efficiency of using VR technology to guide catheterization will create safer treatments for patients and physicians by saving time on one hand and reducing radiation exposure on the other, Monsky noted. These benefits could have further implications for increasing access to catheterization and other cutting-edge interventional radiology treatments for many people in rural settings, who often have limited access to interventional radiology suites and specialists.
"Currently, the lifesaving potential of [interventional radiology] is limited to hospitals and areas with the resources to invest in image-guided technology," he said. "[VR] technology could allow for portability and accessibility so that these procedures are brought to rural areas using nothing more than a suitcase."
The researchers developed this technology through VR startup Pyrus Medical, where Monsky is chief medical officer. They are currently preparing to submit their work to the U.S. Food and Drug Administration (FDA) for approval.