A new automated tool developed at the National Institutes of Health can detect mediastinal and abdominal enlarged lymph nodes more accurately than previous techniques, according to a presentation at the 2014 RSNA meeting.
Depending on how sensitive the software was set to perform versus the number of false-positive detections, sensitivities ranged from 78% at six false positives per volume to about 86% at 10 false positives per volume, reported Dr. Ronald Summers, PhD.
Mediastinal lymph nodes are very important in several kinds of radiology diagnoses, especially in oncology, where either primary lung cancer or metastatic cancers can spread to the mediastinum. Lymph nodes are typically measured using the Response Evaluation Criteria In Solid Tumors (RECIST) criteria, which classify lymph nodes 10 mm and larger as abnormal.
"For lung cancer, it's very helpful to ascertain the precise location of the lymph nodes," Summers said. "The reason it's important is because it determines, to some degree, the surgical approach and method of treatment." The different locations or stations in the mediastinum are numbered in the system developed by the International Association for the Study of Lung Cancer (IASLC), said Summers, who is a senior investigator at the National Institute of Health's Radiology and Imaging Science section.
Summers and his colleagues, principal investigator Joanne Hoffman, Dr. Evrim Turkbey, and Jiamin Liu, PhD, aimed to automatically label lymph nodes in stations by segmenting the organs in the mediastinum. The segmentation information is then used to inform the software as to where the lymph nodes might be sited, Summers said.
The study data consisted of 75 CT scans from 75 patients, five of which served as atlases. In all, there were 316 mediastinal lymph nodes 1 cm or larger, with an average size of 1.6 mm in the short axis. The reference standard was manual labeling by a radiologist.
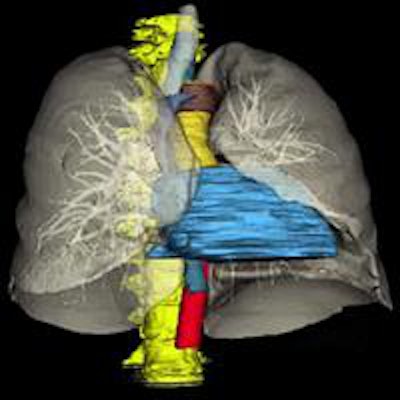
Multiorgan segmentation
The fully automated software identifies eight organs using multiatlas label fusion and the relative position of the node to these organs to assign the IASLC station location.
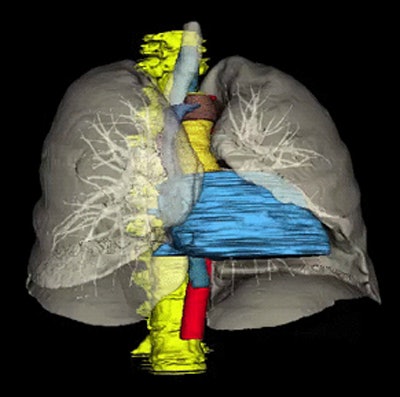 Eight automatically segmented organs include the spine, trachea and lungs, esophagus and aortic arch, pulmonary trunk, ascending and descending aortas, superior vena cava, azygos arch, and heart. All images courtesy of Dr. Ronald Summers.
Eight automatically segmented organs include the spine, trachea and lungs, esophagus and aortic arch, pulmonary trunk, ascending and descending aortas, superior vena cava, azygos arch, and heart. All images courtesy of Dr. Ronald Summers.First is spine segmentation performed using a watershed algorithm that identifies the spine in yellow (the organs are all color-coded). Next comes tracheal and lung segmentations, which use thresholding and morphological operations. Finally, come the other organs, including the esophagus and aortic arch, pulmonary trunk, ascending and descending aortas, superior vena cava, azygous arch, and the heart using the multiatlas technique with joint label fusion, Summers said.
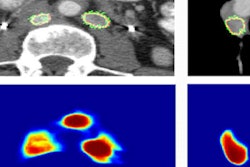
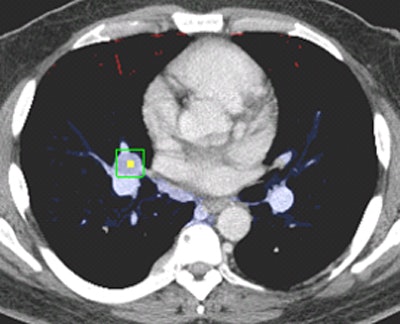 Above and below, examples of correctly stationed lymph nodes.
Above and below, examples of correctly stationed lymph nodes.These atlases are then registered to the target image segment and merged via joint label fusion to generate the final segmentation, Summers said.
How did this complex wave of segmentations perform in identifying lymph nodes?
"Accuracy ranged from a low of 71% in the aortic stations to a high of 88.3% for the inferior mediastinal stations with an average of about 85%," Summers said. There has been some other work as well, so the project is built on the efforts of previous papers by Kensaku Mori, PhD, and William Higgins, PhD, Summers said.
| Performance of lymph node station location vs. radiologists | |||
| Lymph node station | No. of nodes | Correctly labeled | Accuracy |
| Superior mediastinum (stations #2-4) | 123 | 106 | 86.2% |
| Aortic (stations #5-6) |
31 | 22 | 71.0% |
| Inferior mediastinum (stations #7-9) | 77 | 68 | 88.3% |
| Hilar and lobar (stations #10-14) | 85 | 75 | 88.2% |
| Overall | 85.8% | ||
"This method accurately and fully automatically determined mediastinal lymph node stations on thoracic CT," Summers said. "It could be used on lymph nodes detected either automatically by CAD or manually designated by radiologists."
In response to a question from the audience, Summers said that the algorithm has not yet been tried on diseased patients, but it's an important issue, because surgery or severe distortion of the mediastinum can destroy the landmarks the algorithm uses to find lymph nodes.
"One approach is to include such types of images into the atlas, which is worth looking into," Summers said. And even when healthy, "the esophagus can be difficult to segment, because it's a soft, pliable structure that moves around significantly, especially under the carina, where the esophagus tends to weave a little bit more from its vertically oriented course," he said.