The radiology community's proactive response to the adoption of artificial intelligence (AI) offers an important lesson to other clinical specialties in how they should prepare for the new era of AI, according to an editorial published online April 25 in the Yearbook of Medical Informatics.
Rather than resisting change due to fear, the world of radiology has developed an understanding that changes from AI bring not just risks but opportunities, according to Dr. Enrico Coiera, PhD, of the Australian Institute of Health Innovation at Macquarie University in Sydney.
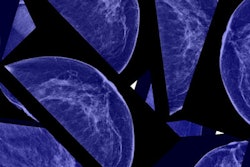
"In the future, radiologists might be freed from working in darkened reading rooms and emerge to become highly visible participants to clinical care," Coiera wrote. "Indeed, in the future, the idea of being an expert in just a single modality such as image interpretation may seem quaint, as radiologists transform into diagnostic experts, integrating data from multiple modalities from the genetic through to the radiologic."
The cost of change
AI will likely yield transformative improvements in efficiency, safety, and clinical outcomes over the next 20 years. But these benefits will come at a cost, he said.
Coiera noted that the highly interconnected nature of healthcare means that changes in one part of the system will require different changes elsewhere. For example, the arrival of cheap bulk AI image interpretation in the future would necessitate modifications to the common reimbursement model of paying radiologists for each image they read, he said. Instead, Coiera noted, the emphasis would be placed on the value of the radiologists' work rather than the volume.
Radiology isn't the only specialty facing new business pressures wrought by AI, however.
"In primary care, for example, the arrival of new, sometimes aggressive, players who base their business model on AI patient triage and telemedicine is already problematic," he wrote. "Patients might love the convenience of such services, especially when they are technologically literate, young, and in good health, but they may not always be so well served if they are older or have complex comorbidities."
As a result, AI-based primary care services might end up caring for profitable low-cost and low-risk patients, with a financially diminished existing primary care system managing the remainder. Coiera suggests a solution to this may again be a shift from volume to value when it comes to radiologist reimbursement.
"Indeed, value-based healthcare might arrive not as the product of government policy but as a necessary side effect of AI automation."
The price of resistance
The different reactions to AI from primary care and radiology offer some important early lessons, according to Coiera.
"One sector is being caught by surprise and playing catch-up to new commercial realities that have come more quickly than expected; the other has begun to reimagine itself in anticipation of becoming the ones that craft the new reality," he wrote.
Each sector pays a different price, Coiera said. He observed that proactive preparation for the future of AI requires investing in reshaping the workforce; actively engaging with industry, consumers, and government; and seriously considering new safety and ethical risks.
"In contrast, reactive resistance takes a toll on clinical professionals who rightly wish to defend their patients' interests, as much as their own right to have a stake in them," he explained. "Unexpected change may end up eroding or even destroying important parts of the existing health system before there is a chance to modernize them."
The practice of medicine is fated to change, and AI will likely be among the biggest change-makers physicians will see in their time, Coiera said. And this change will come with a price.
"What is paid, by whom, and who benefits, all depend very much on how we engage with this profound act of reinvention," Coiera concluded. "To fully engage brings promise of the greatest reward. To not engage is to pay the highest price."