Communicating diagnostic information accurately and efficiently is key to quality patient care. But radiologists continue to create and receive unstructured reports that can compromise diagnosis and treatment.
That's according to Dr. Lionel Cheng and Dr. Bradley Erickson, Ph.D., at the Mayo Clinic in Rochester, MN. They sought to assess whether unstructured follow-up brain MRI reports contained sufficient information for patients' tumor status to be classified, in addition to evaluating the consistency of terms used to describe tumor status in reports. They shared their findings at the 2008 RSNA meeting in Chicago.
"The bulk of radiology reports today are unstructured and contain variations among radiologists, subjective descriptions and interpretation, and incidental findings," Cheng said. "The attitude toward changing the way results are reported is too often, 'Don't fix what isn't broken,' but the reports lack important information."
Cheng and Erickson conducted a retrospective review of consecutive MRI reports for follow-up brain tumor exams performed between January 2000 and December 2007.
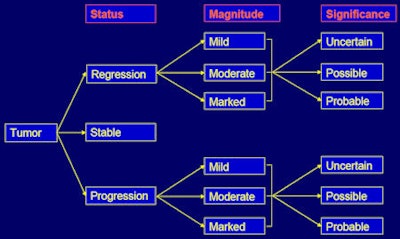
Reports were classified according to the following indicators:
- Tumor status (regression, stable, progression)
- Magnitude of change (mild, moderate, severe)
- Significance of any change (uncertain, possible, probable)
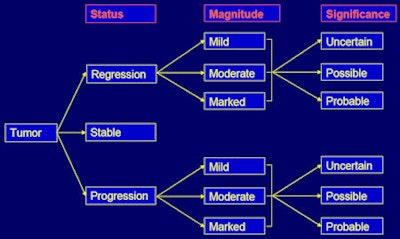 |
| Classification scheme. Image courtesy of Dr. Lionel Cheng. |
"Current tumor classification guidelines are inconsistent," Cheng said. "None are universally accepted, none are uniformly applied, and none cover all three indicators."
For tumor status, the study used the following framework:
- Primary indicator
- Size/volume
- Surrogate indicator such as general statements, signal change, new lesions
- Most recent comparison study
- Multitumor, multilesion studies
- Net change
- "Worse" status
For magnitude, the study used the following terms:
- Mild (mild, slight, minimal, somewhat, small amount, subtle, appears to be some, tiny, partial, slow growth)
- Moderate (moderate, modest, some)
- Marked (marked, significant, clearly, considerable, substantial, pronounced, large amount)
And for significance indicators, the study incorporated the following words and phrases:
- Uncertain (uncertain, slight, subtle, unclear, not entirely atypical of, indeterminate, nonspecific, cannot be entirely excluded)
- Possible (possible, suggestive, benign rather than malignant, may represent, follow-up imaging suggested)
- Probable (worrisome for, suspicious of, concerning for, consistent/compatible with, indicate)
Moderate results
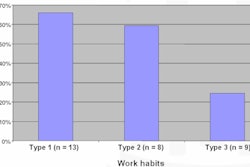
Cheng and Erickson included 238 patients, 778 reports, and 33 radiologists in the study. Six of the 778 reports were unclassifiable. Of the remaining 772 reports, indicators used to classify tumor status consisted of tumor size (27.8%, or 215 reports); other indicators such as enhancement, T2 prolongation, or new lesions (68.7%, or 530 reports); and size (3.5%, or 27 reports).
They found that most unstructured follow-up brain tumor MRI reports contained enough information for tumor status classification. However, almost 1% was unclassifiable, despite reference to prior exams in the report; more than two-thirds of the reports included in the study didn't specify tumor size; and the majority didn't contain data on the magnitude of change when progression or regression had occurred.
The researchers concluded that structured radiology reports could be crucial to ensuring that important indicators of tumor status are communicated clearly to those doctors caring for patients with tumors.
By Kate Madden Yee
AuntMinnie.com staff writer
January 14, 2009
Related Reading
Speech recognition vendors tackle dialect challenges, December 17, 2008
Autofax reporting breakdown spurs Calgary headlines months later, March 19, 2008
Implementing SR before a hospital mandates gives radiology practice upper hand, November 27, 2007
Patience pays off with voice recognition implementation, July 6, 2007
Studies critique radiologists' reports in chest x-ray, knee MRI, April 19, 2005
Copyright © 2009 AuntMinnie.com