PET/CT could be a valuable new imaging technique for distinguishing benign from malignant portal vein thrombosis in liver cirrhosis patients, according to a group in Egypt.
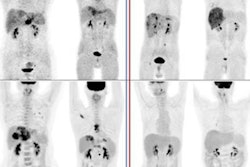
In a small retrospective study, researchers led by nuclear medicine physician Sameh Abokoura, MD, of Menoufia University, found that FDG radiotracer uptake on patient F-18 FDG-PET/CT scans was higher when portal vein thrombi were tumors, rather than benign (or so-called "bland") thrombi.
"Diagnosis of tumor thrombosis and differentiating it from benign thrombosis is essential for managing patients, planning treatments, and minimizing unneeded anticoagulation therapy," the group wrote.
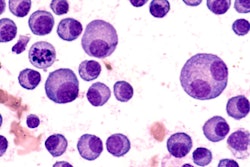
Portal vein thrombosis (PVT) is the complete or partial obstruction of blood flow in the portal vein to the liver due to the presence of a thrombus. Bland thrombi occur in both cancer and noncancer patients; moreover, tumor thrombi and bland can coexist, the authors explained.
While biopsy is the gold standard for differentiating between the two in the clinical practice, combining PET/CT imaging and laboratory results has recently shown promise in establishing a diagnosis in these cases, they added.
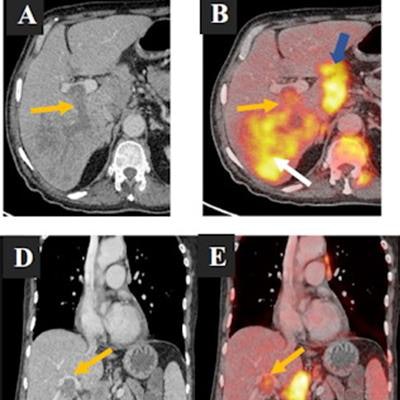
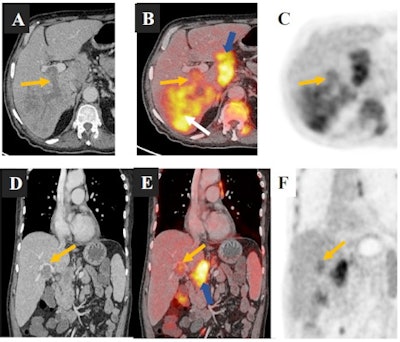 A 67-year-old man with liver cirrhosis and a right hepatic lobe hepatocellular carcinoma (HCC) lesion associated with right portal vein malignant thrombosis. (a-c) Axial contrast-enhanced multi-slice CT (MSCT), axial fused PET/CT, and axial PET images. (d-f) Coronal contrast-enhanced MSCT, coronal fused PET/CT, and coronal PET images revealed linear increased FDG uptake (SUVmax 4) corresponding to right portal vein malignant thrombosis (orange arrows) and increased FDG uptake corresponding to right hepatic lobe HCC lesion (white arrows) and porta hepatis metastatic lymph nodes (blue arrows). Also note increased FDG uptake in the regional spine corresponding to metastatic spinal deposits. Image and caption courtesy of the Egyptian Journal of Radiology and Nuclear Medicine through CC BY 4.0.
A 67-year-old man with liver cirrhosis and a right hepatic lobe hepatocellular carcinoma (HCC) lesion associated with right portal vein malignant thrombosis. (a-c) Axial contrast-enhanced multi-slice CT (MSCT), axial fused PET/CT, and axial PET images. (d-f) Coronal contrast-enhanced MSCT, coronal fused PET/CT, and coronal PET images revealed linear increased FDG uptake (SUVmax 4) corresponding to right portal vein malignant thrombosis (orange arrows) and increased FDG uptake corresponding to right hepatic lobe HCC lesion (white arrows) and porta hepatis metastatic lymph nodes (blue arrows). Also note increased FDG uptake in the regional spine corresponding to metastatic spinal deposits. Image and caption courtesy of the Egyptian Journal of Radiology and Nuclear Medicine through CC BY 4.0.To further explore the role of PET/CT, the researchers analyzed 38 patients who had liver cirrhosis with PVT, either with or without malignant hepatic tumors and who underwent F-18 FDG-PET/CT scans at their hospital in Menoufia between January 2021 and April 2022. For all patients, semiqualitative analysis included data on FDG tracer maximum standard uptake (SUVmax) values.
According to the findings, SUVmax values were significantly higher in the tumor thrombosis group (6.26), compared to the bland thrombosis group (1.79). In addition, with an SUVmax of > 3.5 as a cutoff value, SUVmax achieved a sensitivity of 96.3% and a specificity of 36.4% for distinguishing between the groups.
Ultimately, while PVT is frequently associated with liver cirrhosis, it may also occur in patients with cancer, abdominal sepsis, pancreatitis, systemic lupus erythematosus, or other conditions involving hypercoagulable states, the group noted.
"By using semiqualitative analysis, F-18 FDG-PET/CT is a valuable new technique in differentiating between neoplastic and bland PV thrombi, with optimal cutoff SUVmax value > 3.5 as a criterion," Abokoura and colleagues concluded.
The article was published online June 21 in the Egyptian Journal of Radiology and Nuclear Medicine.