The modern radiology practice continues to experience rapid growth in data, thanks to the ongoing development of imaging modalities and the use of advanced medical imaging in molecular, genomic, and precision medicine. As radiology transitions to value-based care, advanced data analytics is no longer an option.
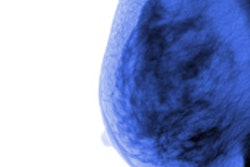
Consider the advances now being made in chronic disease management alone, particularly in cancer treatment. As the density and richness of imaging data continue to improve, it's possible to detect changes resulting from therapies more quickly and with much greater clarity.
Organizations may find it challenging, though, to enhance their capabilities for predictive analytics in support of the American College of Radiology's Imaging 3.0 initiative. It also may be hard to determine when it makes the most sense to keep imaging data locally centralized or physically dispersed.
At the same time that radiology departments are working to improve their workflow productivity, multidisciplinary teamwork, and tools to mine and analyze structured and unstructured data, "Information Generation" patients are asking for faster access to services, personalized experiences, 24/7 access and connectivity, and access on more devices, according to a recent survey of 236 global healthcare leaders conducted by market research firm Vanson Bourne.
Value-based care
How do healthcare providers keep pace with this digital mindset while making the transition to value-based care reimbursement models? Global healthcare leaders have identified a number of top business imperatives they need to deliver against to stay ahead:
- Predictively spot new opportunities
- Population health, value-based care, patient-centered medical home
- Demonstrate transparency and trust
- Treatment options and success rates, access to secure medical records
- Innovate in an agile way
- Clinical research, clinical integration, Internet of Things (IoT)
- Deliver unique, personalized experiences
- 360° patient view, wearables, genomics, precision medicine
- Be always-on, operating in real-time
- Telemedicine, mHealth, medication adherence
Yet only a handful of healthcare providers are addressing these business attributes extremely well or enterprise-wide today. These five business imperatives also have implications for radiology practices as they further link imaging procedures to the accountable care process, where the use of imaging helps with early disease detection and overall hospital length of stay, while contributing to more cost-effective clinical outcomes through optimizing radiation dose and demonstrating exam clinical utility.
 Roberta Katz from EMC.
Roberta Katz from EMC.Despite the myriad challenges in front of them, the stage is set as healthcare leaders work to modernize their IT infrastructure through the application of next-generation predictive analytics. Utilizing big-data analytics at the point of care brings together diverse data points from across the continuum to improve operational efficiencies, accelerate care collaboration, and focus on the overall patient life cycle.
However, there's still much work to be done. In fact, 81% of respondents to the 2015 Healthcare Information and Management Systems Society (HIMSS) Leadership Survey still had basic questions about the quantity and type of data they should be collecting, and how to best turn that data into insight.
Given that many legacy IT infrastructures often lack the analytic capabilities to make timely insights, this number is not surprising. Meeting the needs of the Information Generation and taking healthcare into the future will depend on healthcare providers making the journey to a modern data center -- bringing analytics, data, and applications together.
What are the next steps? How can radiologists effectively support their empowered patients through the use of next-generation predictive analytics?
Diving into data lakes
Enter the "data lake" concept, which provides an effective, modernized framework to consolidate, optimize, and analyze healthcare data, helping to bridge the gap between raw data and actionable insight. This IT infrastructure uses traditional and next-generation access methods to incorporate information from internal and trusted external data sources across the health system, including payors, public health databases, genomic research centers, biobanks, and even social media feeds.
Data are ingested, catalogued, inventoried, and controlled regardless of the source or destination. This powerful architecture provides a unified location across the healthcare ecosystem to reduce silos and provide massive scalability, multiprotocol data-in-place analytics, and enterprise data protection.
Large databases of patient images and text can also be pooled into the data lake for further mining and analysis by clinical departments, business analysts, and data science teams. With the enhanced ability to derive business and clinical value through analytics, healthcare providers can drive forward accountable care initiatives, creating a new realm of data science for uncovering trends, patterns, relationships, correlations, and discoveries that can truly impact integrated patient care.
Also, using a data lake builds on your current analytics investments and helps simplify storage, management, and analysis through integration of data in real-time, near real-time, or in batches from disparate sources -- without affecting day-to-day operations or access to data. Analytics can become forward-looking with the ability to incorporate images from multiple service lines including radiology, cardiology, pathology, and dermatology to further impact quality care improvements.
The 6 steps to success
As healthcare organizations work more broadly to build a modern and agile IT infrastructure as cost-effectively as possible, radiology departments can employ predictive analytics to gain a more holistic patient perspective as they find, curate, and govern data. This enables continuous improvements in operational efficiencies such as imaging volume and turnaround times, clinical outcomes, and patient engagement.
But will greater investments in predictive analytics and data lakes actually deliver? The numbers say yes: 54% of health IT leaders who spent 1% to 5% of their operating budget on analytics reported success within financial and clinical management, according to a report from Deloitte. A 2015 Goldman Sachs study also projected that digital health initiatives could yield total savings upward of $305 billion.
As healthcare organizations work to transform to a modern data center and incorporate the next generation of predictive analytics, EMC recommends a series of best practices to ensure success:
- Develop a long-term big-data analytics strategy mapped to priorities and budget.
- Identify where analytics can add value, help achieve business and clinical goals, and improve technology and organizational structure.
- Create a vision for the future where data analytics becomes a core organizational strategy.
- Identify the right first opportunity, prioritize potential use cases, and capture initial, critical data sources.
- Develop a proof-of-value project.
- Align business, clinical, and IT requirements to optimize the infrastructure.
What we once considered the future of healthcare is here today. Organizations must determine how they keep pace with accelerated rates of innovation, meet today's healthcare challenges, and successfully shift to value-based care. Using advanced analytics to achieve these objectives and provide next-generation care delivery will be the key differentiator among healthcare providers in this highly competitive landscape.
Roberta Katz is director of EMC Healthcare Solutions.
The comments and observations expressed herein are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.