While radiologists differ in their ideas for creating an optimized display of 2D and 3D images, consensus default display protocols (DDPs) can produce a high level of agreement, according to a multi-institutional research team.
Contending that neither radiologists nor PACS diagnostic workstation designers have seriously dealt with the need to design DDPs for 2D and 3D images, a team of researchers from the Hospital of the University of Pennsylvania (HUP) in Philadelphia, the Baltimore VA Medical Center (BVAMC), and the University of Maryland Medical Center in Baltimore initiated a formal study to evaluate DDP preferences for 2D and 3D by a group of radiologists.
Dr. William Boonn, a chief radiology resident at HUP, presented the results of his colleagues and fellow researchers at the International Society for Optical Engineering (SPIE) Medical Imaging conference, held earlier this year in San Diego.
PACS vendors have failed to keep abreast of the surge in simultaneous viewing of both 2D and 3D images at a time when an increasing number of high-volume CT procedures are mandating the use of advanced visualization, according to the researchers.
For example, radiologists review more than 90% of all the CT examinations performed at the BVAMC in volumetric mode, irrespective of the indication. Clinicians review 25% of the CT scans in volumetric mode.
Today's workstations have semi-integrated functionality, with 2D and 3D interpretation being launched in separate windows, according to the researchers. This functionality allows a user to open a study in a 3D application without needing to search or use a work list.
However, any changes or manipulations made in the 3D viewer are not propagated back to the 2D system in the PACS. When 3D models are created, no manipulations can be made after a 3D screen capture is transferred to the PACS for static viewing.
The lack of full integration results in reduced efficiency because of the need to switch back and forth between different applications, Boonn said.
Because productivity can be aided or hampered by the types and locations where images are displayed, the research team evaluated the default display preferences of radiologists with 18 standard CT protocols performed at BVAMC. The protocols were based on body part and indication with or without prior exams and with or without contrast administration.
The eight radiologists represented different specialties and levels of experience. Their hanging preferences for CT images had been previously observed by the research team.
Each radiologist was given blank sheets of paper on which to draw preferred display protocols for both 2D and 3D images on a workstation configured with two grayscale monitors and one color monitor. Dr. Khan Siddiqui, chief of imaging informatics and cardiac CT/MR imaging at BVAMC, said that if the study was conducted again, the radiologists would instead be given the option of using three high-resolution color monitors.
The objective of the study was to identify similarities and recurring patterns in each of the 18 protocols evaluated, and create a consensus DDP format for each protocol that would be acceptable to the majority of participating radiologists. While there was a large variance in the initial "blank slate" evaluation, consensus layouts led to a high level of agreement, according to the researchers.
The most surprising result was the near unanimous desire to use a 4:1 configuration on the grayscale monitors, said Dr. Nabile Safdar, a musculoskeletal radiologist at the University of Maryland Medical Center.
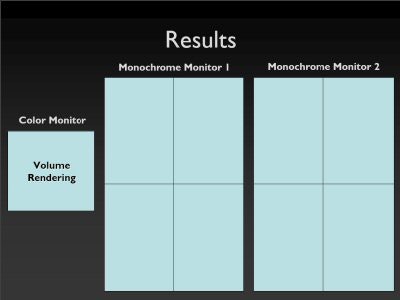 |
| Consensus 4:1 display protocol on grayscale monitors. Image courtesy of Imaging Informatics Section, Department of Radiology, Baltimore VA Medical Center. |
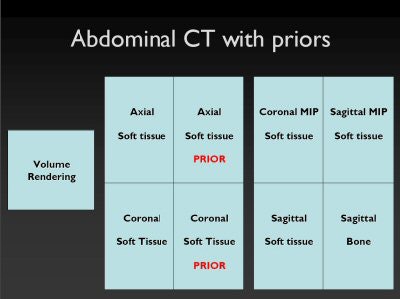
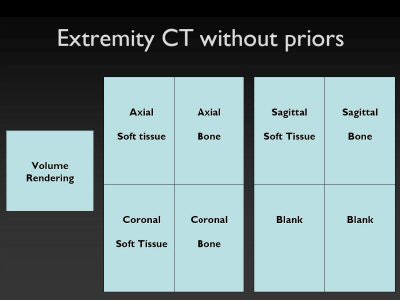
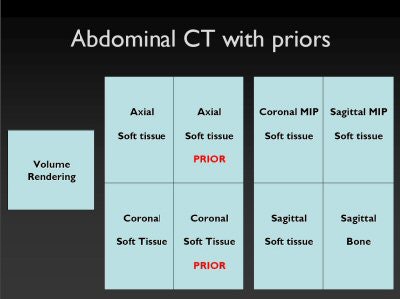
Other consistent findings included the display of images in all three planes (axial, sagittal, and coronal), images displayed in multiple window/level settings, and specialized 3D applications, such as lung window multiple intensity projection (MIP) images to look for lung nodules on chest CT scans, or angiography window MIP images on CT angiograms for vessel analysis.
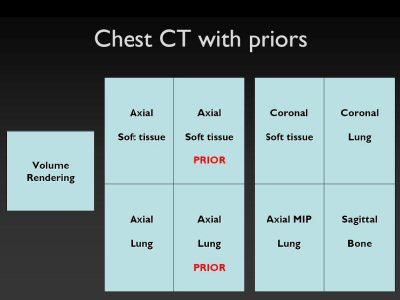 |
| Consensus display protocols for chest CT with priors, extremity CT without priors, and abdominal CT with priors, respectively. Images courtesy of Imaging Informatics Section, Department of Radiology, Baltimore VA Medical Center. |
 |
 |
The research team believes that this simple exercise can help define radiologists' preferences for 2D and 3D image display that can be used by PACS vendors as guidelines for the creation of DDPs when tightly integrated workstations are created.
"While it is typical for radiologists to customize DDPs, they want a starting point to work from," Safdar said. "The starting point should be the most optimal display for the average radiologist."
Consensus formats offer the benefit of providing input from radiologists, and can be a standard that both 3D software vendors and PACS workstation vendors can follow, Boonn said.
"Rather than have vendors develop a DDP format for radiologists, it is much better if radiologists quantify their preferences for display of specific imaging protocols," Siddiqui said. "More of these simple tests using different protocols should be conducted."
Sadfar observed that neither tight integration nor establishing DDP formats that please the majority of viewers will be easy. He pointed out that the audience for each intended display protocol may differ.
"Radiologists will be using 3D for primary interpretation," he said. "Clinicians, such as orthopedic surgeons, also will open the same study and not be as comfortable in the axial plane."
Safdar believes that DDP evaluation research needs to be conducted with different types of radiology practices and with groups of other clinical specialists.
"Vendors need to get the input of cardiologists, neurosurgeons, and orthopedic surgeons," he said.
Ideally, when these specialists log into the next generation of intelligent PACS workstations, the DDP protocols developed for their specialty will be displayed as well as the toolbox designed for their level of expertise.
"Our research project is just a starting point," Boonn said.
By Cynthia Keen
AuntMinnie.com contributing writer
June 12, 2006
Related Reading
3D CT measures accurately for total knee arthroplasty, May 31, 2006
3D ultrasound bring efficiency gains, May 25, 2006
Technologists take advantage of 3D opportunity, April 25, 2006
Part 1: Automated CT lung nodule assessment advances, April 17, 2006
Expanded role looms for 3D in breast imaging, April 11, 2006
Copyright © 2006 AuntMinnie.com