Capturing CT radiation dose information is a hot topic, but it's complicated by the incomplete methods used for measuring, determining, and calculating dose, said Anthony Seibert, PhD, of the University of California, Davis. Seibert discussed dose capture in a January 25 webinar hosted by the Society for Imaging Informatics in Medicine (SIIM).
Without appropriate correction factors that account for patient body size, current radiation dose indicators -- CT dose index volume (CTDIvol) and dose-length product (DLP) -- can't be reliably used as measures of patient dose, Seibert said. Estimation of organ dose and the use of age- and gender-specific risk coefficients are also necessary to determine a patient's risk.
"It is tempting but incorrect to use simplified approaches such as effective dose for determining individual patient doses and [associated] risk from CT studies," Seibert said.
Getting CTDIvol and DLP
Radiation dose indicators CTDIvol and DLP can be obtained from a dose summary page, which includes information about the CT exam. They can also be provided by a DICOM Radiation Dose Structured Report (RDSR), but not all scanners are capable of producing these reports, Seibert said.
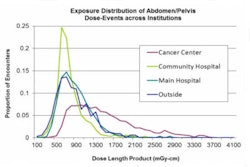
Blindly reporting CTDIvol and DLP as the radiation dose, however, can cause problems, he said. For example, there's a mismatch between patient body size and the size of CT phantoms that serve as the basis for CT scanner calculations of CTDIvol.
"When you scan different parts of the body, the accumulation of these indices is inappropriate," he said.
CTDIvol does allow the comparison of scan protocols or scanners and is useful for obtaining benchmark data to compare techniques, but it's not so good for estimating patient dose. CTDIvol conversion factors are needed due to differences in patient size.
"A patient who is scanned with a body acquisition technique and the 32-cm-diameter volume phantom that's used to calculate or estimate what the CTDIvol is certainly is going to have differences compared to that of the shape of the body," he said.
As an added complicating factor, some scanner manufacturers may use a 16-cm-diameter phantom to estimate CTDIvol for pediatric bodies, while others may use the 32-cm-diameter phantom.
DLP, an indicator of the dose imparted to the patient, is calculated by multiplying CTDIvol times the scan length. In addition to being affected by the issues associated with CTDIvol, DLP can be problematic in a limited scan range, according to Seibert.
It would be desirable to have a magic single number, i.e., effective dose, Seibert said. However, the conversion factors that convert DLP to effective dose are also problematic due to the body size mismatch and other factors. Although it's not intended for individual patient dose metrics, effective dose can be a reasonable surrogate for a population measure, he noted.
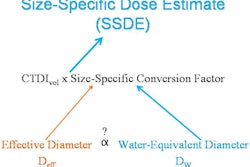
Medical physicists are working to make the CTDIvol indicator a better measure of patient dose. For example, Task Group 204 of the American Association of Physicists in Medicine (AAPM) has developed size-specific dose estimates in pediatric and adult CT exams in an attempt to make these measurements more accurate, he said.
The task force found that CTDIvol can be normalized by using a lookup table of conversion factors derived from the diameter of the phantom on which the scanner's CTDIvol was based.
Seibert said that it's also misleading to associate an estimate of effective dose with any specific patient without any of the necessary corrections to CTDIvol and, ultimately, DLP.
California dose reporting law
In the fall of 2010, California passed a radiation dose reporting law, SB 1237. It has three sections that require CT scanner users to report dose:
- Section 115111 covers dose reporting from CT and will take effect on July 1, 2012.
- Section 115112 covers accreditation and is required by July 1, 2013.
- Section 115113 addresses reporting of high doses from CT and radiation therapy and is mandatory by July 1, 2012.
As of July 1, a facility conducting CT exams must electronically send CT studies and protocol pages that list the technical factors and radiation dose (defined as either CTDIvol and DLP or the dose unit as recommended by the AAPM) to the PACS. With CT systems that are capable of calculating and displaying the dose, the dose information needs to be included in the radiology report, or the protocol page needs to be attached to the report.
"The problem is that not all scanners are capable of sending the [DICOM] radiation dose structured report, and it would be nice to electronically integrate with the radiology report," Seibert said. "So there's a lot of effort on being able to do this to be able to meet the letter of the law."
Doing it right
As described by Michael McNitt-Gray, PhD, of the University of California, Los Angeles, dose reporting capabilities are currently at phase 0 on the path toward performing this process correctly, Seibert said. Radiologists today can meet the letter of the law in California by manually dictating the CTDIvol and DLP from the protocol page for each of the individual series into the radiology report.
It's unclear, though, whether it's appropriate to provide a summary of CTDIvol and DLP. "To accumulate the CTDIvol and DLP is perhaps not correct," he said.
In phase 1, which is partially achieved, the dose information from DICOM radiation dose structured reports can still be manually dictated into the radiology report.
"Some scanners create the DICOM [radiation dose] structured report, but it's not always easy to read and dictate," Seibert said.
The goal is to reach phase 2 by July 1, 2012, he said. In this phase, the appropriate values from the DICOM structured report will be automatically inserted into the radiology report.
Phase 3 will incorporate dose information adjusted by body region and patient size, automatically inserted into the report. More sophistication will follow in phase 4 with the addition of accumulated organ doses, according to Seibert.
Additional capabilities will follow in phase 5. "There's a lot of room for expansion and improvement," he said.
University of California efforts
The University of California is pursuing a dose reporting initiative, moving, for example, toward providing reporting of organ doses and other body-size-adjusted doses, Seibert said.
The University of California, Davis is also working on its own dose reporting process.
"What we're trying to do independently is to take the DICOM dose structured report from the CT scanner, send the dose page to the PACS, but also send the radiation dose structured report to an interface engine," Seibert said. "[The engine] then extracts the information, packages it into an HL7 message that will go to our radiologist dictation [system], and our radiologist dictation report will have the CTDIvol and the DLP inserted automatically. It'll then be sent to our RIS and, ultimately, to our electronic medical record."
Initially, CTDIvol and DLP will be presented as an accumulated dose. Ultimately, however, the goal is to have the dose indicators available on a series-by-series basis, he said.
Seibert added that the institution believes a disclaimer should be used, given the problematic nature of the CTDIvol and DLP dose indicators.
"The bottom line is, if there are questions with respect to these types of studies, a medical physicist should be consulted," he said.