SmithGroup, Inc.
Bill Rostenberg, Morris Stein of The Stein-Cox Group in Phoenix, and Dr. Steven Horii from the University of Pennsylvania in Philadelphia will lead a refresher course (No. 624) at the 2002 RSNA meeting. "The Digital Department: Its Architecture and Design" will take place on December 5, 8:30-10 a.m., Room E353B.
Proper workflow is the key to efficient facility planning. Work patterns and the highly repetitive movement of staff between different activity areas is a major driver of facility layout.
In the old days, facility layout revolved around the film processor. Traditional film-based imaging facilities were typically planned with rooms of diminishing importance placed within concentric circles around the dark room (figure 1). Those requiring short foot travel to and from the dark room were placed closest; those for whom film-cassette travel was of less importance were placed more distant. The advent of daylight processors enabled slightly more decentralized facilities, but workflow still reflected film-cassette traffic.
 |
| A traditional dark room-centered layout where the workflow revolves around the film processor and dark room. |
Digital imaging systems have done much to rewrite the rules of imaging facility planning. Today’s challenge is to coordinate the various types of workflow, both physical (footsteps) and virtual (electronic transmission), while integrating enterprise-wide operations. Several distinct types of flow must be considered: patients, personnel, information, and supplies.
Patient flow
Patient flow will vary depending on whether your facility treats outpatients, inpatients, or a combination. Inpatient procedure rooms should be placed with good access to inpatient elevators and gurney holding areas. Direct access to the emergency department (ED) is essential for critical emergency modalities, such at CT. If imaging is too far from the ED, these modalities will have to be duplicated in the ED, which can be costly.
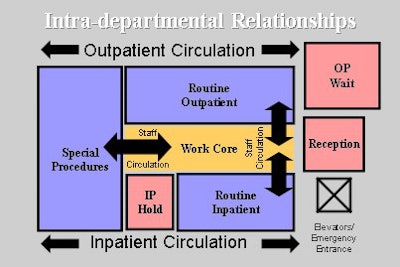
Where inpatients and outpatients are treated, separate corridors should be considered so ambulatory persons do not need to pass patients in gurneys (figure 2). When patient volume is unusually high, a room in one zone can be used for the other population, thus permitting flexible use of rooms, while maintaining the separation between the two types of patients.
 |
| A facility that treats inpatients and outpatients should consider intradepartmental relationships. Ambulatory patients should not need to pass by patients in gurneys, but procedure-room placement should be flexible enough to accommodate either type of patient. Images courtesy of Bill Rostenberg. |
All facilities should have short-duration and high-volume procedure rooms (i.e. dedicated chest imaging rooms) that are located toward the front-entrance side of the facility. Longer-duration, lower-volume procedure rooms (interventional suites) should be located toward the back. In this way, traffic flowing through the department is kept to a minimum, and inappropriate traffic is kept away from interventional areas.
Personnel flow
Internal traffic patterns to consider involve radiologists, technologists, radiologic nurses and support staff. While digital imaging practices enable decentralization of functions, some physical adjacencies remain critical. A work-core configuration (see figure 2) that separates staff and patient traffic is still a valid planning model, although less work-core area is required for digital processes. Adequate support space for clean supplies and equipment, and clean-up functions, should be close by to avoid unnecessary repetitious foot traffic. Storage for frequently used supplies should also be provided in each procedure room.
Although soft-copy reading rooms can be located anywhere, it is wise to place them with good access to interventional procedure rooms, where the radiologist must be present during procedures. Ideally, reading areas should be small enough to afford acoustic and visual privacy, yet large enough to allow several radiologists to collaborate on difficult cases.
Reading areas placed adjacent to a small conference room allow radiologists to move to the conference area for larger rounds without having to leave the reading zone. Some provisions should be made for referring-physician consultations within the reading zone without disturbing private reading areas.
Flow of information
The greatest impact of digital imaging on facility planning is on information flow. Images from CT, MRI, and other modalities have been transmitted electronically for some time now. Many organizations are now converting from plain-film modalities to electronic acquisition and distribution.
Ten years ago, a central digital archive required 600-800 square feet of space, a raised computer floor, and an industrial-type air conditioning system. The archive typically took up valuable hospital space.
Today, less space is required. No computer floor is necessary, and ventilation requirements are similar to those of a general office space. Archives are often remotely located in less-valuable construction, or are contracted out, eliminating the need for dedicated space.
Dark rooms and film file-room areas are becoming unnecessary with digital imaging. A "master plan" should be developed to assure that once these spaces are vacated, they are used for functions appropriate to their location. Some institutions aggressively transition from film to digital imaging; others evolve more slowly. Keep in mind that hybrid phases of development -- in which both soft copies and hard copies are used -- are costlier to operate and more space-intensive to house. Interim phasing plans should identify how the facility can support these operational stages while minimizing disruptive construction.
Supply flow
Electronic imaging processes obviously reduce the need for film and chemistry, but don’t don’t necessarily eliminate it. Regardless of whether images are acquired on film or digitally, clean supplies must be brought in and soiled goods must be removed. As interventional modalities grow, so does the need for "surgical" supply and distribution systems. This means providing sink alcoves, allocating space for case-cart storage, and designing "controlled" corridors for interventional rooms similar to those employed in surgical suites.
Common obstacles
Room utilization is commonly measured in terms of procedures per day (or month/year) per room. Sometimes it is measured in terms of income per procedure room per day, month, or year. One obvious way to increase room utilization is to extend the hours of operation, but this also increases operating expenses.
Roadblocks to efficient room utilization unnecessarily increase procedure turnaround times. For example, if dressing rooms and gowned waiting areas are remote from the procedure room, the staff must spend additional time "hunting" for patients, thus reducing room utilization. The same is true when staff must scavenge for supplies from distant utility rooms.
Another example of poor room utilization is a lack of space, such as having a toilet room that can only be accessed through a dressing room or a dressing room that can only be exited through a procedure room.
Interventional procedures generally require patient preparation, holding, and recovery spaces. Too often, patients are held in corridors because adequate holding areas have not been provided. This is not only a poor practice; it often violates building codes and licensing requirements. Using the procedure room as a default holding area can significantly reduce utilization.
Several institutions are co-locating interventional procedure rooms with surgical operating rooms. This concept provides appropriate controlled circulation for interventional activities, and allows specialized recovery staff to care for a variety of patients needing medical observation, pre-procedure preparation, and post-procedure recovery. Efficient patient preparation and/or recovery have a direct impact on improving procedure-room utilization.
By Bill RostenbergAuntMinnie.com contributing writer
November 18, 2002
Portions of this article are adapted from The Architecture of Imaging by Bill Rostenberg.
Bill Rostenberg is a vice president in the San Francisco office of SmithGroup, Inc. Architects and Planners (www.smithgroup.com). He is the author of Facility Design for Medical Imaging Workstations and Design Planning for Freestanding Ambulatory Care Facilities. Rostenberg is a fellow of the American College of Healthcare Architects and the American Institute of Architects. He is a guest instructor on health facility design at the Harvard University Graduate School of Design, professional development program, in Cambridge, MA, and the Clemson University graduate program in architecture and health in Clemson, SC. Rostenberg can be contacted at 415-365-3463 or at [email protected].
Related Reading
Facility-planning implications of the new MRI safety guidelines, September 9, 2002
MRI design resonates with functional, aesthetic qualities, July 22, 2002
Finding the right space for a new imaging center, July 15, 2002
Copyright © 2002 AuntMinnie.com



















