The National Coalition for Quality Diagnostic Imaging Services (NCQDIS) welcomes the additional flexibility that the U.S. Centers for Medicare and Medicaid Services (CMS) has brought to the Stark Laws. The new regulatory exceptions and modified interpretations should facilitate Stark compliance for a variety of common contracting arrangements. Phase II also clarifies many of the ambiguities identified in public comments following issuance of the Phase I Rule.
However, a substantial loophole remains in the statute with regard to the in-office ancillary services exception, which currently allows non-radiologist physicians to install imaging equipment in their offices and bill for the imaging services regardless of whether they have received formal training in its utilization.
It is the position of NCQDIS that the current incarnation of the physician self-referral law does not address this form of in-office self-referral, and that if left in its current state, this loophole will leave the door open to potentially gross abuses of the statute.
When initially proposed in the early 1990s, exemptions to federal self-referral and antikickback laws seemed reasonable compromises that respected the sanctity of physicians' autonomy in their practices. The exemptions gave physicians latitude in investment options, but only when those investments would not have undue influence on care delivery. Similarly, before the advent of expensive imaging techniques or widespread use of diagnostic procedures such as colonoscopy, self-referral for ancillary services would likely have been limited to laboratory testing or other low-cost services.
However, these self-referral and safe-harbor exemptions currently are not effective in restraining physicians' financial interests from influencing care. Advances in medical technology and practice have transformed the in-office ancillary-services exemptions into potentially lucrative opportunities for physicians.
The broadened clinical applications of modalities such as MRI have increased their potential to boost patient volume, making investment in such equipment feasible for non-radiologist physician practices. Physicians' strategies threaten to raise costs for public and private payors through overutilization of these diagnostic imaging services (Health Affairs, March-April 2004, Vol. 23:2, pp. 70-81).
Self referral equals higher costs
An article in The New York Times (March 13, 2004) pinpointed non-radiologists in Syracuse, NY, as the source of higher utilization and increased healthcare costs in that area. Instead of referring patients to a radiologist, doctors installed MR scanners and other medical imaging equipment in their offices and performed the imaging themselves -- a practice that NCQDIS and a multitude of others in the diagnostic imaging community recognize as a form of self-referral (American Journal of Roentgenology, October 2002; Vol. 179:4, pp. 843-850).
NCQDIS has observed that physicians who acquire their own MRI or CT scanners create a very high-fixed-cost business that requires them to image a significant number of patients each day just to break even on the equipment investment. In addition, in-office self-referral increases the amount of money a physician can make, creating an irresistible urge to order as many tests as possible (Health Affairs, March-April 2004, Vol. 23:2, pp. 70-81).
Blue Cross Blue Shield has said that diagnostic imaging costs in the U.S. are expected to total nearly $100 billion annually by 2005, a 25% increase from the $75 billion paid in 2000 (Blue Cross and Blue Shield Plans Respond to Challenge of Keeping Medical Technology Affordable press release, October 14, 2003).
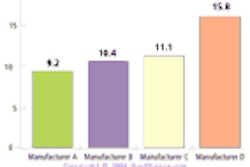
For its part, the Medicare Payment Advisory Committee (MedPAC) has said that diagnostic imaging is increasing more rapidly than any other medical service, with a 9% average annual growth in Medicare spending for diagnostic imaging since 1999 (Variation and Innovation in Medicare, June 2003, MedPAC report to Congress).
In his May 5, 2004, testimony to the subcommittee on health of the Committee on Energy and Commerce, MedPAC chairman Glenn Hackbarth said that growth rates were more than 15% per year for services such as MRI, CT, and nuclear medicine.
NCQDIS has come across a number of studies published in the medical literature that show that when in-office self-referral opportunities exist in imaging, higher utilization is the inevitable result. For example, two studies showed that in a series of common clinical scenarios, self-referring physicians ordered between two and eight times as many imaging tests as physicians who referred their patients to radiologists (Journal of the American Medial Association, October 1992, Vol. 268:15, pp. 2050-2054; New England Journal of Medicine, December 1990, Vol. 323:23, pp. 1604-1608).
In 1994 the U.S. General Accountability Office (formerly the General Accounting Office) conducted a similar investigation, and found that self-referring physicians performed between two and five times as many imaging tests as those who referred their patients to radiologists (Referrals to Physician-Owned Imaging Facilities Warrant HCFA’s Scrutiny, October 1994, GAO/HEHS-95-2, pp. 1-62).
Who's imaging?
A 2003 study showed that between 1993 and 2001, the noninvasive diagnostic imaging utilization rate per thousand Medicare beneficiaries remained essentially flat among radiologists, whereas it rose by 33% among nonradiologists (Radiology, September 2003; Vol. 228:3, pp. 795-801).
What this means is that essentially all the growth in utilization of imaging in recent years is attributable to nonradiologist physicians who operate their own imaging equipment in-office. It is quite clear from the published evidence in the medical literature that self-referral is the most important cause of the rapid increases in utilization rates of diagnostic imaging that have occurred in recent years.
But it appears that changing the system is possible. The Maryland Health Occupations Article §1-301 (k) (2) enacted in 1993 prohibits self-referral in much the same manner as the Stark law -- but with a notable difference.
The statute provides that "except for a radiologist group practice or an office consisting solely of one or more radiologists, 'in-office ancillary services' does not include: (i) magnetic resonance imaging services; (ii) radiation therapy services; or (iii) computed tomography scan services." This language reflects a legislative intent to prohibit referrals for in-office MRI tests or CT scans, unless the equipment is owned by a practice made up entirely of radiologists.
The Maryland State Legislature cited academic studies that showed that the three pieces of imaging equipment excluded from the in-office ancillary services exception were where the most instances of abuse take place. For this reason, they deemed that with regard to the provision of high-end imaging procedures, it was in Maryland's best interest for diagnostic imaging to be performed by those physicians formally trained in the practice of radiology.
The point the Maryland State Legislature was trying to make is this: a radiologist has to have diagnostic imaging equipment in his or her office. It is a requirement. It's what radiologists were trained to do -- perform scans and interpret the findings for other doctors.
Physicians in other fields of medicine cannot say the same. After four years of medical school, doctors choose the fields of medicine in which they wish to practice and subsequently receive extensive training in that area of medicine during their residency program. It seems counterintuitive and potentially harmful to both patients and the healthcare system for a physician to practice a field of medicine in which he or she did not receive formal instruction.
By Cherrill FarnsworthAuntMinnie.com contributing writer
July 20, 2004
Farnsworth is executive director of NCQDIS, a Washington, DC-based professional organization that represents more than 2,400 outpatient diagnostic imaging centers and departments in the U.S. Through affiliated professional societies, the NCQDIS message reaches over 150,000 centers and professionals involved in providing diagnostic imaging services. Visit the NCQDIS Web site for more information.
Related Reading
The impact of phase II Stark regulations on freestanding imaging centers, May 13, 2004
Due diligence builds imaging center muscle, December 19, 2002
Final rules bar doctors from profiting on Medicare "self-referrals", January 4, 2001
U.S. fraud and abuse rules create a minefield for imaging vendors, August 31, 2000
Copyright © 2004 NCQDIS