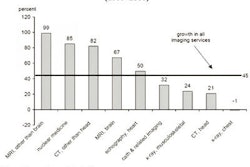
In response to double-digit increases in diagnostic imaging procedures, Massachusetts healthcare insurers are implementing imaging management plans in an effort to curb utilization. Last year, Harvard Pilgrim Health Care of Wellesley, MA, which covers 822,000 lives, instituted an imaging review policy administered by radiology benefits management firm National Imaging Associates (NIA) of Hackensack, NJ.
Recently, Tufts Health Plan of Waltham, MA, which covers 747,000 lives, reported that it, too, would be incorporating an imaging review policy to be administered by NIA on October 1 this year. This was followed up last week by the announcement that Blue Cross Blue Shield of Massachusetts (BCBSMA), the state's largest private healthcare provider with 2.7 million members, would be establishing a high-end diagnostic imaging preauthorization policy beginning December 1 this year.
The plan calls for "high utilizers" of certain imaging procedures to undergo a clinical review of their imaging requests, according to Chris Murphy, media relations manager for BCBSMA. "Lower utilizers," according to Murphy, will not have their high-end imaging requests undergo clinical review, but will have to register their imaging order with the healthcare provider's radiology benefits administrator, American Imaging Management (AIM) of Deerfield, IL.
Murphy declined comment on the specific thresholds of what constituted low- and high-imaging utilization, and how the payor arrived at that determination, for BCBSMA providers.
Neepa Patel, vice president of business development and marketing for AIM, said that the imaging utilization review plan was still being refined prior to implementation by BCBSMA. However, she said, the plan does not call for a review of the use of all radiology modalities -- just those deemed high-tech by the company.
"The BCBSMA program focuses on high-tech imaging," she told AuntMinnie.com. "So that's MRI, CT, PET, and some nuclear cardiology procedures."
In addition to imaging requests by BCBSMA primary care providers, in-office ancillary imaging services conducted by nonradiologists within the BCBSMA network will be under the AIM imaging review process plan, as well imaging orders by all its subspecialty providers, such as cardiologists and oncologists, according to Patel.
Although unable to provide specifics of the proposed BCBSMA imaging review plan, Patel offered an overview of AIM's radiology benefits management.
"We have a set of proprietary guidelines that are radiology-specific around high-tech imaging that are used to determine the medical appropriateness of an exam for a particular patient," she said.
The firm created its guideline criteria through the use of material from various clinical societies, such as the American College of Radiology, the Society of Nuclear Medicine, and the American College of Cardiology, as well as from research published in peer-reviewed medical journals, she said.
The appropriateness criteria are embedded into an information system that is accessible via the Web or via a call-in center for AIM's clients. Physicians enter the patient's history and the type of imaging study that they wish to order for the patient into the decision matrix. About 80% of the requests for imaging exams are approved, according to Patel.
In some cases, there is not enough patient information provided to accurately assess the request. In these instances, the firm will have a nurse contact the physician office for clarification. About 5% of the time, Patel said that AIM will have one of its physician reviewers contact the requesting physician to discuss the case under consideration.
"They'll have a collegial discussion about what they're trying to do with the exam and whether that is the most appropriate exam to order," she said.
The physician reviewers are board-certified in cross specialties, such as radiology, cardiology, and internal medicine, Patel said. They are also further trained in the specifics of radiology management, she noted.
Murphy said that BCBSMA will not reject a physician request for an imaging study, and that the role of the forthcoming plan is to provide an expert source of advice for its healthcare providers.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
September 12, 2005
Related Reading
Thousands taking unneeded health tests -- U.K. doctors, August 24, 2005
MedPAC, Medicare, and imaging growth, August 16, 2005
National health expenditures and another year of 'unsustainable growth', May 4, 2005
ACC, ACR debate stats on imaging growth, April 18, 2005
ACR criteria cut imaging costs in Israel, January 11, 2005
Copyright © 2005 AuntMinnie.com