WASHINGTON, DC - Most radiologists polled in a recent survey agree that peer review is an important component of any quality assurance initiative. But most would rather see peer review conducted anonymously, according to a study presented Monday at the American Roentgen Ray Society (ARRS) annual meeting.
In a survey of staff radiologists at Sunnybrook Health Sciences Centre at the University of Toronto, a majority of respondents believed that peer review is important for improving patient care (86%) and professional development (81%). However, the vast majority (92%) also believed that peer reviews should be anonymous, in part, so they don't have an adverse effect on working relationships.
"Further investigation about radiologists' attitudes and perceptions about formal peer-review systems in general is important, not only for determining their potential effect on patient care, but also radiologists' relationships and psychology in the workplace," said lead study author Dr. Michael Loreto, an abdominal imaging fellow at Sunnybrook.
Reducing errors, improving quality
Over the past decade, radiology departments seeking to improve quality assurance have used various forms of peer review as a means to identify and reduce errors, which have significant implications further down the healthcare chain.
"Medical error represents a significant source of patient morbidity and mortality, as well as financial cost to the healthcare system and individuals," Loreto added. "With the increased reliance placed on radiology in the past several years, errors made by radiologists can have significant implications on patient outcomes, as well as related costs."
Sunnybook is the second-largest hospital in Toronto and employs 39 staff radiologists. Until recently, the facility used an informal method to review radiologists' work, relying on individual radiologists to voluntarily discuss errors among each other and at quarterly departmental morbidity and mortality rounds, Loreto said.
In the fall of 2012, Sunnybook introduced a formal peer-review program, which was integrated into the hospital's PACS (Agfa HealthCare). The PACS randomly selects 3% of cases to evaluate.
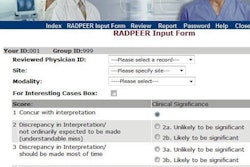
The new program isn't anonymous, however, which allows colleagues to review a study and provide a retrospective evaluation. That assessment, which uses a grading system similar to that of RadPeer from the American College of Radiology, is then submitted online. Major discrepancies also are discussed quarterly by section and departmental heads.
The name of the radiologist who originated the report is disclosed, but he or she is not privy to the reviewers' names.
Before the implementation of the program, an anonymous 26-question survey was distributed to Sunnybrook's staff radiologists. The questions were designed to assess the knowledge, attitudes, and perceptions of peer review in general and the new Sunnybrook system in particular, Loreto explained.
The questionnaire was returned by 36 of 39 staff radiologists, with broad representation of all subspecialties, as well as a fairly good range of experience among the radiologists in the department, he added.
Program benefits
Survey results found a strong preference for making peer-review programs anonymous. In all, 92% of respondents preferred anonymous peer review, with 86% adding that nonanonymous methods adversely affect the objectivity of the evaluator. In addition, 58% did not believe they could be unbiased when reviewing a case reported by someone with whom they had a close working relationship.
Also, 74% of those polled were concerned about the potential malpractice implications of peer review, and 67% thought peer review had the potential to damage personal relationships in the department. What's more, 42% of the respondents felt there was a possibility that a poor review could affect their job security or department ranking.
"Interestingly, this [result] was a concern held among senior radiologists in the department," Loreto said.
The poll found that an overwhelming majority of respondents thought the new peer-review program was beneficial, and 86% replied that the evaluations improve patient care. In addition, the majority (81%) agreed that the assessments were important to their own professional development.
Whereas the previous review method at Sunnybrook required voluntary disclosure of errors, 81% of respondents said they routinely would advise their colleagues if they noticed a misdiagnosis and an error, while 19% said they would not point out mistakes. Most of those radiologists who would decline to mention errors were the less experienced readers, with less than 10 years on the job.
A follow-up question asked whether radiologists felt "equally comfortable" disclosing errors made by fellow radiologists with more or less experience than themselves. Approximately one-third said they did not feel comfortable mentioning the errors, with 53% of readers with less than 10 years of experience among the uncomfortable critics.
Similarly, more experienced radiologists (94%) were more likely to advise a colleague of an error than their less experienced colleagues (68%).
Negative impact
Loreto and colleagues noted the potential for peer-review programs that aren't anonymous to have adverse effects. Among the respondents, 75% thought a peer-review program would take time from their workday and affect department workflow. However, an overwhelming majority thought the program would be minimally intrusive, requiring less than three hours per week.
Among the conclusions reached by Loreto and colleagues is that formal peer-review systems "are necessary to ensure participation amongst all members of the department, especially amongst less experienced staff who may have some trepidation about participating in an informal system."