
In-person consults between radiologists and acute care surgeons led to changes in medical and/or surgical planning in approximately 40% of cases, according to a study published in the August issue of the Journal of the American College of Radiology.
The findings suggest that, in an era where electronic medical record systems and PACS allow for the instant delivery of data across health systems, face-to-face contact definitely has its place, said corresponding author Dr. Matthew Davenport of the University of Michigan Health System.
 Dr. Matthew Davenport from the University of Michigan.
Dr. Matthew Davenport from the University of Michigan."With the advent of electronic communication, the way referring physicians interact with radiologists has changed dramatically," he told AuntMinnie.com. "But we know that some content and nuance is lost in electronic or text-based communication, and this can have an effect on patient treatment. When you're talking with a surgeon directly, it creates this real-time back and forth that's very helpful."
Let's talk
In 2015, lead author Dr. Elliot Dickerson and colleagues established semiweekly rounds of about 60 minutes in length between the on-call acute care surgery team and one of three abdominal radiologists. During these meetings, an attending surgeon outlined the current diagnostic impression and treatment plan before the group performed a comprehensive imaging review of the primary radiologic examination. Over the course of the year, 100 cases were reviewed, the most common of which were CT of the abdomen and pelvis with contrast (83 of 100 cases).
Radiologists could ask for clarification regarding the history of the patient as well as how the surgical team planned to use imaging study information to develop a plan; surgeons could ask questions of the radiologists as well. After each patient discussion, the attending radiologist reviewed the original radiology reports and revised his or her recommendation if necessary. The attending surgeon was also asked to state the postreview diagnostic impression and treatment plan (JACR, August 2016, Vol. 13:8, pp. 943-949).
The results were dramatic. Dickerson and colleagues found that these face-to-fact consults led to changes in both surgeons' diagnostic impressions and in medical/surgical planning in 43 cases, or 43%. Forty-seven percent of these were changes in acute management (20 of 43) and 44% resulted in changes in operative management (19 of 43).
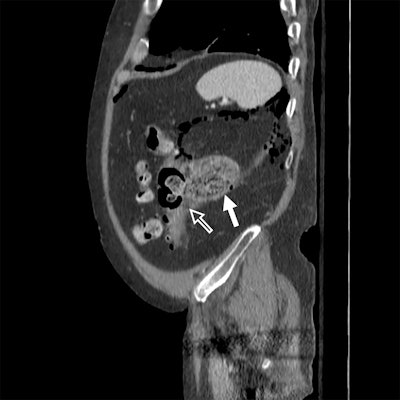 Sagittal (above) and axial (below) contrast-enhanced CT images of the abdomen and pelvis are from a 62-year-old man with abdominal pain. Images show a large collection posterior to the descending colon (white arrow) containing feculent material adjacent to multiple diverticula and a sizeable defect in the colon wall (hollow arrow). The initial management strategy was percutaneous drain placement; however, from the conference, the surgical team learned that the size of the defect was much larger than they had realized. The patient underwent descending colectomy with transverse colostomy. Images courtesy of Dr. Matthew Davenport.
Sagittal (above) and axial (below) contrast-enhanced CT images of the abdomen and pelvis are from a 62-year-old man with abdominal pain. Images show a large collection posterior to the descending colon (white arrow) containing feculent material adjacent to multiple diverticula and a sizeable defect in the colon wall (hollow arrow). The initial management strategy was percutaneous drain placement; however, from the conference, the surgical team learned that the size of the defect was much larger than they had realized. The patient underwent descending colectomy with transverse colostomy. Images courtesy of Dr. Matthew Davenport.Why did the consults make such a difference? In-person communication may improve mutual understanding in a variety of ways, such as clarifying radiology test characteristics (for example, sensitivity or positive predictive value), or uncovering medical or surgical history that may have been buried in a patient's report. It could also provide a clearer sense of the clinical issue to be resolved, as well as give the referring physician a better understanding of the meaning of the radiology report, the group wrote.
The impact face-to-face meetings had on treatment planning was surprising, Davenport said.
"The effect of these meetings was much larger than we expected," he said. "A change rate of roughly 40% -- that's shockingly high."
Communication barriers?
What hinders interaction between radiologists and other physicians? In addition to the lack of reimbursement for time spent reviewing patient records in person, it's difficult for physicians to carve out space in their schedules for these types of meetings, Davenport said.
"We only have so many hours in the day, and, unfortunately, when an activity isn't reimbursed it's hard for physicians to make the time," he said. "Even if an activity shows patient benefit, it's difficult. This is a common theme uncovered by quality improvement research, that fee-for-service payment models actively encourage suboptimal care patterns."
Yet research that has tracked radiologist participation in these kinds of multidisciplinary meetings has found improved morale, a better sense for physicians of positively affecting patient care, and a decrease in feelings of isolation.
"Each meeting necessitated approximately one to two hours of attending radiologist effort and approximately one hour of effort from all other attendees," Dickerson and colleagues wrote. "However, there was multidisciplinary recognition of the apparent impact this activity was having on patient care and heightened sentiments of teamwork and camaraderie."
The bottom line is that this kind of research points the way forward as the delivery of healthcare shifts from quantity to quality, according to Davenport.
"Our study is another example of how we know what we should be doing -- even if we're not always following through," he said. "Hopefully as healthcare delivery continues to shift from quantity to quality, there will be more support for this kind of collaboration."




















