The American College of Radiology has weighed in on the U.S. Centers for Medicare and Medicaid Services (CMS) proposed Medicare Physician Fee Schedule (MPFS) 2025 rule.
The organization noted that the CMS expects the overall impact of the proposed MPFS to be neutral on radiology, nuclear medicine, and radiation oncology. However, interventional radiology will have a decrease of 2%.
In the rule, the CMS estimates a 2025 conversion factor of $32.36 compared to last year's $33.29 (calculated by removing the 1.25% provided by the Consolidated Appropriations Act of 2023 that applied to services furnished January 1 through March 8 of this year and a 2.93% payment increase provided by the Consolidated Appropriations Act of 2024 that will be applied to services provided March 9 through December 31 of this year and by applying a positive 0.05% budget neutrality adjustment), the ACR said.
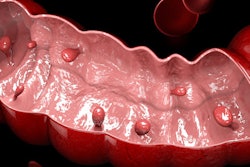
The college was pleased, however, with the proposed rule to provide coverage of colorectal cancer screening with CT colonography (CTC), replacing double contrast barium enema.
"ACR applauds this proposal as a big step forward toward providing Medicare patients access to a minimally invasive CRC screening tool that can detect pre-cancerous polyps and does not require anesthesia," it said.
The ACR also highlighted the following:
- The CMS plans to accept the Relative Value Scale Update Committee (RUC) recommended values and physician times for radiology-related codes, including six new MRI safety codes.
- It is flagging several potentially misvalued services, including CPT code 27279 (arthrodesis, sacroiliac joint, percutaneous or minimally invasive); 10021 (fine needle aspiration biopsy, without imaging guidance, first lesion); 10004 (fine needle aspiration biopsy, without imaging guidance, each additional lesion); 10005 (fine needle aspiration biopsy, including ultrasound guidance, first lesion); and 10006 (fine needle aspiration biopsy, including ultrasound guidance, each additional lesion).
- It reports that the American Medical Association (AMA) expects to complete its new Physician Practice Information Survey (PPIS) analysis and document by the end of 2024 and will be sharing the data with the CMS when it becomes available.
- The CMS has introduced a new request for information that builds on the Merit-based Incentive Payment System (MIPS) Value Pathways (MVPs) framework to improve ambulatory specialty care.
- The agency plans to keep category weights for the MIPS program the same as those from 2022: Quality, 30%; cost, 30%, promoting interoperability, 25%, and improvement activities, 15%.
- The ACR noted that the CMS has made changes to how the quality category is scored in an effort to ease difficulties some specialties, including radiology, face "due to the increasing number of measures being removed from the program or capped at seven points." The proposal would include all "topped-out" diagnostic radiology measures (i.e., 360, 364, 405, and 406) and would finalize the removal of measure 436 (Radiation Consideration for Adult CT --Utilization of Dose Lowering Techniques), replacing it with measure 494 (Excessive Radiation Dose or Inadequate Image Quality for Diagnostic CT in Adults).
The college said it expects to release a detailed summary of the proposed rule in the coming weeks.