Radiologists have seen tremendous changes to their practice in the last 25 years, more than in any other medical profession. Topping the list are technological changes, which have brought a multitude of new procedures that were hardly conceivable two decades ago. There have also been significant decreases in reimbursement, which the entire medical field has had to contend. The cuts have occurred in both the fee-for-service and managed care fields.
A dramatic shortage of radiologists has emerged as a third major trend. Reasons for the shortage are unclear, but it seems that not enough new radiologists are entering the profession to replace those who are retiring. Some may be discouraged by the complexity of the technology, others by the specialty's bureaucracy, and some by the changes wrought by declining reimbursement.
As a result, radiology faces a very difficult problem -- how to provide quality patient care in the midst of a severe staffing shortage.
Many groups have stepped forward to try to move into or even force their way into radiology, subverting the traditional role of radiologists as the guardians of imaging technology. General practitioners are installing their own x-ray machines, OB specialists are placing ultrasound equipment in their offices, and specialists from cardiologists to orthopedic physicians are installing imaging equipment in their facilities. ER physicians, nurse practitioners, and physician assistants are also trying their hand at imaging.
All is not lost in radiology, however, as a number of facilities are actively seeking solutions to the provider crisis. One such institution, Weber State University in Ogden, UT, has developed a potential solution under the guidance of Jane Van Valkenburg, Ph.D. The university's radiology practitioner assistant (RPA) program is unique in many ways, and could potentially help relieve the radiologist shortage faced by institutions across the U.S.
The RPA is a physician extender, not a physician replacement, and is a mid-level health professional in radiology. For years, I have taught radiologic technologists that they are the eyes and ears for the radiologist. Now Weber State has taken the concept a step further. The program takes registered technologists with a minimum of five years' experience, providing the academic background and clinical experience they will need to become competent mid-level professionals in radiology.
Students work with board-certified radiologists for 1,200 hours of clinical time to develop the skills and experience required to perform imaging procedures. Most students who enter the program are certified in more than one area of medical imaging, which helps them in the program. However, multiple credentials are not required for acceptance. All applicants, however, must be an RT(R), (ARRT), or certified in radiography.
An RPA enhances patient care and allows the radiologist to be more productive and efficient by providing more time to be spent on the time-consuming task of image interpretation. Utilizing an RPA also prevents the entry of nonradiology personnel into the field, because the RPA always works under the supervision of the radiologist.
An RPA may perform 15 to 20 procedures daily, and can average 300 procedures a month. A typical workday for an RPA might involve performing all of the GI barium studies, perhaps a biopsy or a fluid drainage, and an arthrogram or two. And the RPA might assist the radiologist with vascular examinations. In essence the RPA would do whatever the radiologist directs him or her to do, but a radiologist is always present during procedures, and dictates the final reports.
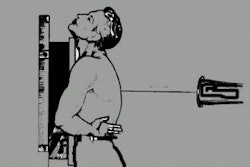
An RPA is also capable of performing many of the routine tasks the radiologist now performs, such as fluoroscopy procedures, evaluating cases by separating normal from abnormal, conducting patient assessments, interacting with patients, and performing minor invasive procedures.
Previous experience enables the RPA to work cooperatively with the technologists and radiologists to maintain quality patient care and efficiency within the department. An RPA can spend more time with patients, providing them with instructions and explanations prior to a procedure and afterwards. An RPA essentially provides patients with the personal contact that radiologists don't have the time to give. Healthcare facilities spend much money on committees to develop patient awareness and on educational materials, but fail to realize that most patients want someone to discuss procedures with them face-to-face.
The RPA is a product of an intense educational program and works as an extension of the radiologist, similar to the relationship between the PA and GP. RPAs recognize that they are not licensed physicians and realize their limitations. They are, however, trained registered technologists who have completed two-year academic programs and 1,200 hours of clinical experience that demonstrates their competency in performing procedures to qualify for the certification examination offered by the Certification Board for Radiology Practitioner Assistants. Upon successfully passing the examination, they may use the RPA credentials in recognition of their accomplishments. The starting salary range for an RPA is from $60,000 to $80,000, plus benefits.
The world of radiology should recognize the manpower resource within the profession and utilize the RPA to their full potential. Otherwise, they must be prepared to see non-radiology professionals continue to erode the very world they call home.
By John W. LarsenAuntMinnie.com contributing writer
October 25, 2001
John Larsen, CBRPA, has been working in radiology since 1964. He is employed by Kent Radiology and is an RPA for Trinity Hospital, both in Grand Rapids, MI. He can be reached at [email protected].
Related Reading
Radiology job market looks rosy in coming years, October 15, 2001
RTs take home more money in 2001, July 2, 2001
Radiologic sciences offers diverse career opportunities, June 22, 2001
Copyright © 2001 AuntMinnie.com