After many years of using conventional fluoroscopic evacuation proctography, or defecography, radiologists at London's University College Hospital have switched over entirely to MR proctography for imaging of the pelvic floor. Fluoroscopy is only used when a patient has a contraindication to MRI.
"I have been won over to the extent that now I am not too sure that the fluoroscopic technique has any significant advantages over MRI," said Dr. Steve Halligan, noting that MRI's lack of ionizing radiation is critical in a group of patients comprising mostly young women.
At Friday's special focus session, the clinical rationale behind the change to MR was explained. In a recent prospective study conducted at University College Hospital, researchers compared the clinical utility of both techniques. Results showed that when clinicians (coloproctologists, urogynecologists, and gastroenterologists) were asked to declare whether they had a preference for either MRI or fluoroscopy, MRI was the clear winner. The fact that MRI is not performed in the physiological position (i.e., sitting down) did not appear to have a material impact on its clinical value.
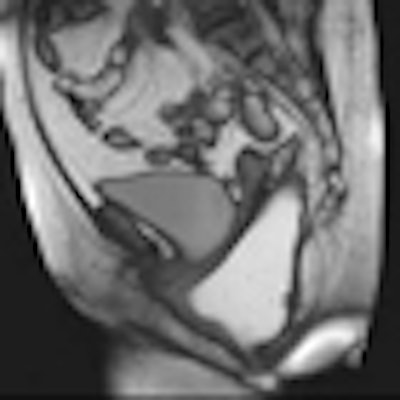
 Sagittal late evacuation view shows a cystocele in the middle and posterior pelvic floor compartment. Image courtesy of Dr. Steve Halligan.
Sagittal late evacuation view shows a cystocele in the middle and posterior pelvic floor compartment. Image courtesy of Dr. Steve Halligan.
The concept of moving over to MRI might seem daunting, but in reality the change is easy and radiographic technicians have adopted the MR technique enthusiastically, according to Halligan. Fluoroscopic methods require a single cine sequence at rest, and again while voiding, which is obtained in the sagittal plane (steady-state precession gradient echo -- e.g., TrueFISP). This provides all required information about the position of the pelvic floor and pelvic organs at rest and during evacuation, and it also provides an assessment of the completeness and difficulty of voiding, if any.
Dynamic pelvic MRI can match the performance of the fluoroscopic technique, but there are other possibilities. For example, the integrity of pelvic floor muscles is well demonstrated by MRI, unlike fluoroscopy, and this may provide useful clinical information, although the precise role for MR still needs to be defined.
While the effects on continence of anal sphincter damage following childbirth are well established, the contribution made by damage to other pelvic floor muscles is not yet completely understood. Halligan expects to see clarification of this area over the next few years. Moreover, MR can afford the opportunity to make spectroscopic measurements from the pelvic floor musculature, and this may have clinical benefits, although this is very much work-in-progress.
Pelvic floor disorders may be difficult to diagnose and are usually evaluated by combining different clinical and radiological investigations, explained Dr. Francesca Maccioni of the department of radiological science at the University "La Sapienza" in Rome. Dynamic MRI has emerged as an alternative method of imaging in the evaluation and understanding of disorders of the pelvic floor, due to its multiplanar capability, high soft-tissue contrast and adequate temporal resolution.
Speakers at Friday's session discussed how MRI can demonstrate the main dysfunctions of the posterior pelvic floor, and also outlined current clinical indications and implications of dynamic MRI of the pelvic floor. A major advantage of MRI is that it provides a unified view of the pelvic floor, and diseases of the anterior, middle, and posterior pelvic floor compartment can be adequately assessed in a single examination. It can also help to reduce examination time, costs, and patient discomfort, but importantly it provides a highly accurate and noninvasive evaluation of a unitary system that is often assessed and treated separately. Furthermore, because dynamic MRI offers a complete evaluation of the posterior anorectal compartment and of the anterior and middle compartments, urogynecologists and proctologists can be assisted with their clinical diagnosis, according to Maccioni.

 Left: MR image obtained at rest, after rectal filling with gel; normal values of anorectal angle and anorectal junction, with respect to the pubococcygeal line. Right: MR image obtained during straining and evacuation: A large anterior rectocele develops, associated with descent of the posterior pelvic floor. Images courtesy of Dr. Francesca Maccioni.
Left: MR image obtained at rest, after rectal filling with gel; normal values of anorectal angle and anorectal junction, with respect to the pubococcygeal line. Right: MR image obtained during straining and evacuation: A large anterior rectocele develops, associated with descent of the posterior pelvic floor. Images courtesy of Dr. Francesca Maccioni.While the examination is neither painful nor particularly disturbing, Maccioni believes that possible causes of discomfort may be related to claustrophobia, the use of a rectal contrast medium, and attempting tricky maneuvers under unfavorable conditions. It can be difficult, in a closed magnet unit and in the supine position, to attempt functional maneuvers, and sometimes this may be unhygienic, she added. MRI techniques should be further developed to reduce possible discomfort, and her suggestions for doing this include thorough explanations to patients about the procedure. It is critical because the success of dynamic MRI derives from the effectiveness of the maneuvers performed, she stated.
Maccioni would also like to see the wider use of dedicated open magnets to allow the examination to be performed in a seated position. In addition, she favors the use of high-field MRI (3 tesla) to boost understanding of the physiopathologic basis underlying these diseases. The use of MR tractography to detect neural abnormalities and the use of MR spectroscopy for a more detailed analysis of muscular abnormalities underlying some pelvic dysfunctions are of particular interest.
She expects that historical boundaries between different specialists will be broken down, as a multidisciplinary approach develops. Pelvic floor clinical units, based on teams of experienced physicians, surgeons, and radiologists, will become increasingly widespread in the future, she predicted.
Originally published in ECR Today March 4, 2011.
Copyright © 2011 European Society of Radiology