When it comes to breast imaging, some mistakes are more common than others. They can broadly be categorized as detection or interpretation errors, and are primarily affected by the patient's mammographic density and tumor type, the technology, and personal skills, noted Dr. Eleanor Cornford, consultant radiologist at the Nottingham Breast Institute in Nottingham, U.K.
Depending on the clinical setting, the reader is likely to operate at different levels of mammography sensitivity and specificity, which affects errors.
"In a screening setting there is the necessity to work at slightly lower levels of sensitivity to achieve acceptable levels of specificity, whereas when faced with a patient with a symptomatic problem, attention is also paid to more benign appearing features," she said.
To reduce false-negative errors, Cornford recommends increasing conspicuity of cancers to enable improved detection, training and education to improve interpretation, and following guidelines to aid optimum assessment of mammographic abnormalities. She also recommends comparing current imaging with previous imaging, and for radiologists to audit their work.
Mammography is not the only place where errors occur: Breast MRI sees its fair share as well. Use of the modality is on the rise due to its sensitivity and specificity; however, technical difficulties in association with a lack of expertise in reading breast MR exams can lead to misinterpretation and errors, according to Dr. Federica Pediconi from the department of radiological sciences at the University of Rome "La Sapienza" in Italy.
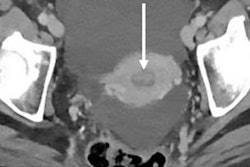
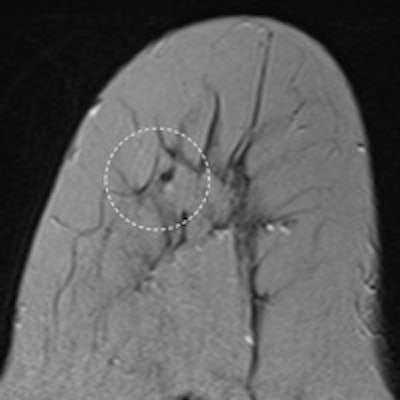
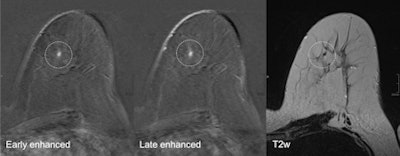 A 52-year-old patient who had breast cancer five years previously. MRI detected focus in the left craniomedial breast called BI-RADS 4, and a second opinion was requested. All images courtesy of Dr. Pascal Baltzer.
A 52-year-old patient who had breast cancer five years previously. MRI detected focus in the left craniomedial breast called BI-RADS 4, and a second opinion was requested. All images courtesy of Dr. Pascal Baltzer."Breast MRI is technically demanding, requiring excellent fat saturation, high spatial resolution, and rapid performance of postcontrast sequences," she said. "Common causes of false-positive diagnoses are represented by artifacts that can be related to the patient or to technical parameters."
Other factors of imaging interpretation error can be related to the presence of background parenchymal enhancement that can reduce the diagnostic accuracy and insufficient history or lack of practice in reading MR images. During her presentation, Pediconi will provide an overview of different types of diagnostic errors as well as the way to avoid them and handle them.
Errors in second-look ultrasound after breast MRI also are quite common. Every finding detected by MRI classified greater than BI-RADS 2 has to be worked up through follow-up or biopsy, which can be done by MRI (as that was the method detecting the lesion). But this is expensive and in many cases not possible as most radiologists doing breast MRI do not provide a biopsy unit, according to Dr. Pascal Baltzer from the department of radiology at the Medical University of Vienna.
The next choice is ultrasound: cheap, broadly available, and easy to apply once it's known where the lesion is located, he said. Outside of research papers, ultrasound and second-look ultrasound are not differentiated -- most ultrasound examinations are targeted to mammographic or clinical findings and could be called targeted or second-look ultrasound.
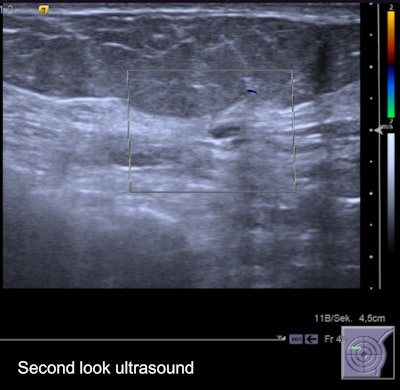 Second-look ultrasound of the lesion. It's an oval, horizontally oriented lesion with circumscribed borders, posterior acoustic enhancement, and no hypervascularization. Internal features unspecific hypoisoechoic. It was found to be probably benign on ultrasound, and followed up over two years without evidence of growth.
Second-look ultrasound of the lesion. It's an oval, horizontally oriented lesion with circumscribed borders, posterior acoustic enhancement, and no hypervascularization. Internal features unspecific hypoisoechoic. It was found to be probably benign on ultrasound, and followed up over two years without evidence of growth."We all do a lot of examinations; most of them we do not immediately get feedback from," he said. "I heard doctors from the German screening program brag, calling their sensitivity 100% -- that is of course they see the cancers they detect, not the ones they miss. Regarding second-look ultrasound, it is similar and a lot of things can be taught: How often do I find a correlate for MRI lesions? Can I also see nonmass lesions? Can I upgrade or downgrade lesions using ultrasound? What lesions am I likely to miss and can I do anything about it?"
Baltzer anticipates an increased use of ultrasound in breast imaging, particularly to determine whether lesions can be upgraded or downgraded by ultrasound and whether ultrasound follow-up is possible in MRI-detected lesions. Empirical evidence is lacking, in spite of the many examinations done everywhere, he added.
"I guess this is because you can faster measure and publish data connected to 'fancy' topics such as diffusion-weighted imaging -- the latter being a helpful but only additional technique that is scientifically largely overrepresented as compared with second-look ultrasound," he said. "Second-look ultrasound after breast MRI is -- or should be -- everyday practice in every breast unit."
Baltzer's talk will aid delegates in the practical application, limitations, and pitfalls in second-look ultrasound.
At today's session, ECR delegates will learn about mistakes in mammography, breast MRI, and second-look ultrasound after breast MRI -- as well as how to reduce the frequency of their occurrence. Nobody will want to miss it, because as Cornford points out: "The only people that don't make mistakes are those that do no work!"
Originally published in ECR Today on 3 March 2016.
Copyright © 2016 European Society of Radiology